Mammography is a specialized medical imaging technique that uses low-dose X-rays to create detailed images of the breast. It plays a critical role in the early detection and diagnosis of breast cancer, helping to identify tumors and tissue changes long before physical symptoms appear. A mammogram, the image produced during mammography, allows radiologists to evaluate breast health and detect potential abnormalities with precision.
This article explains what mammography is, how it works, and the different types available, including screening and diagnostic mammograms, digital mammography, and 3D mammography (breast tomosynthesis). It also addresses common concerns such as breast compression, radiation exposure, and image accuracy, while outlining when and how often mammograms should be performed. Below is an overview of the mammography procedure:
- Patient preparation: Includes scheduling, hygiene guidelines, and medical history.
- Clothing removal: Wearing a gown and removing upper-body garments and jewelry.
- Proper positioning: Positioning the breast for standard imaging angles.
- Breast compression: Flattening the breast to improve image clarity and reduce radiation.
- Image acquisition: Capturing multiple images using low-dose X-ray technology.
- Post-imaging procedure: Immediate post-exam care and return to routine activity.
- Image evaluation and results: Radiologist interpretation and follow-up guidance.
Understanding these steps can help patients feel more informed and comfortable during the process, while emphasizing the importance of regular breast screening in maintaining long-term health.
Key Takeaways
- Mammography is a vital medical imaging technique that uses low-dose X-rays to detect breast cancer and other abnormalities, classified into screening and diagnostic types.
- The mammography procedure involves patient preparation, proper positioning, compression of breast tissue, and thorough evaluation of images by radiologists to ensure accurate results.
- Regular mammograms are recommended to begin at age 40, with specific guidelines for frequency based on age and risk factors, emphasizing the importance of early detection of breast cancer.
What is mammography?
Mammography is a specialized type of medical imaging that uses low-dose X-rays to produce detailed images of the breast. Its primary purpose is to detect and diagnose breast diseases, particularly breast cancer, at an early stage, often before physical symptoms appear. By capturing internal views of breast tissue, mammography can identify small tumors, calcifications, and other abnormalities that may not be felt during a physical exam. There are two main types of mammography:
- Screening mammograms are conducted on women without any symptoms, serving as a routine preventive tool.
- Diagnostic mammograms are performed when symptoms such as lumps, pain, or nipple discharge are present, providing more focused and detailed images to aid diagnosis.
Mammography is also commonly referred to as breast X-ray, breast imaging, or simply a mammogram. Regardless of the term used, its goal remains the same: to support early detection and improve the chances of effective treatment and recovery.
Is mammography radiology?
Yes, mammography is a branch of radiology. Radiology is a medical specialty that employs imaging techniques to diagnose and treat diseases within the body. Mammography specifically uses low-dose X-ray technology to create detailed images of the breast tissue. These images help radiologists, who are medical doctors specializing in interpreting medical images, to identify any abnormalities in the breast that may indicate the presence of breast cancer or other breast diseases.
The American College of Radiology (ACR) sets the standards for conventional mammography practices, ensuring that mammography facilities adhere to high-quality imaging protocols and maintain a lower radiation dose.
The use of advanced technologies such as digital mammography and 3D mammography (digital breast tomosynthesis) has further enhanced the accuracy and effectiveness of breast cancer screening. These technologies provide clearer images and reduce the likelihood of false-positive results, minimizing unnecessary stress and additional testing for patients.
Can mammography detect breast cancer?
Yes, mammography can detect breast cancer, but it’s important to understand that it is not foolproof. Mammography is highly effective in identifying early signs of breast cancer, such as abnormal masses or calcifications in the breast tissue. However, it is not definitive. If a mammogram reveals suspicious areas, further testing, such as a breast ultrasound or a breast biopsy, is often required to confirm the diagnosis.
The ability of mammography to detect breast cancer depends on various factors, including breast density and the size of the tumor. Dense breast tissue can sometimes obscure the presence of tumors, making them harder to detect. This is why additional imaging methods, such as digital breast tomosynthesis or breast MRI, are sometimes recommended for women with dense breasts.
Despite these limitations, regular screening mammograms are a crucial tool in the early detection of breast cancer and early-stage cancer, significantly improving the chances of successful treatment and survival. A screening exam can further enhance this process.
How does a mammography work?
A mammogram, the medical imaging test used in mammography, works by using low-dose X-ray technology to create high-resolution images of the internal structures of the breast. The primary aim is to detect early signs of breast abnormalities, including cancer, when they are most treatable.
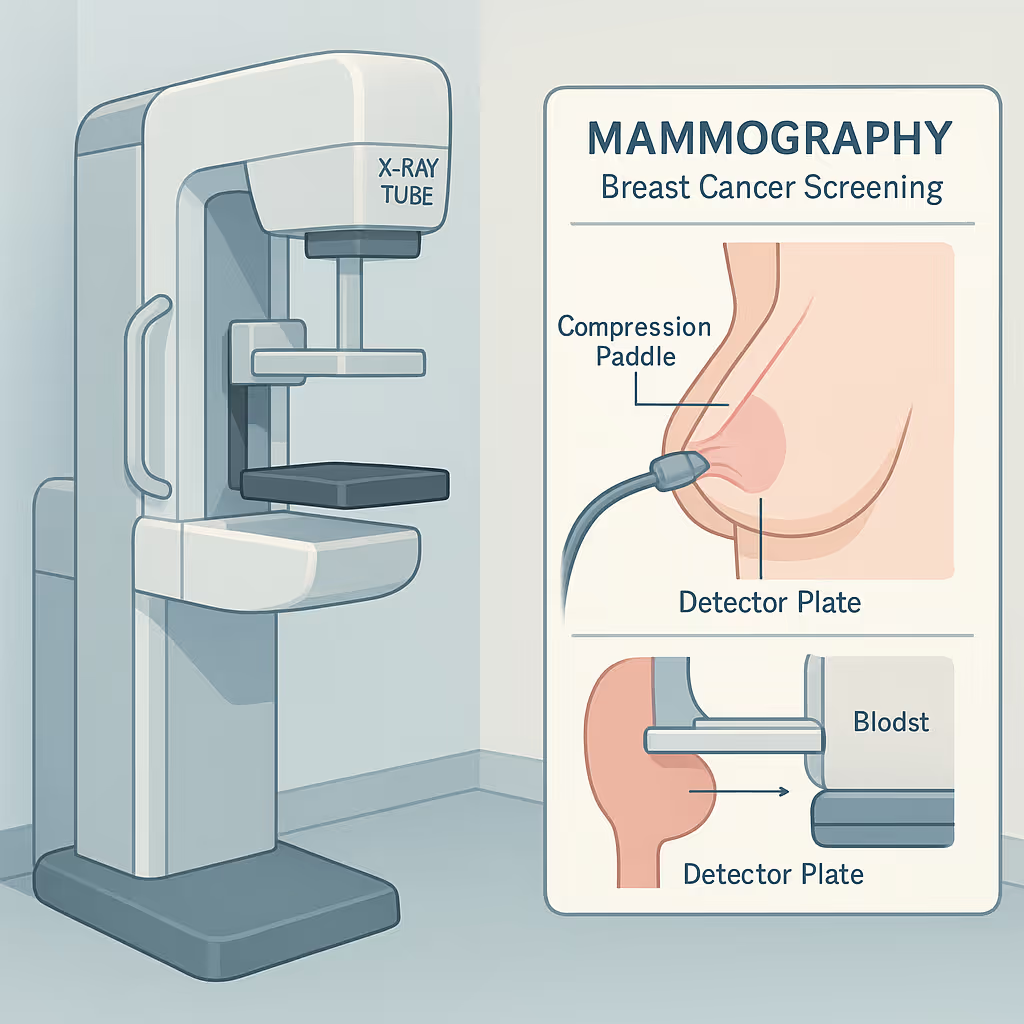
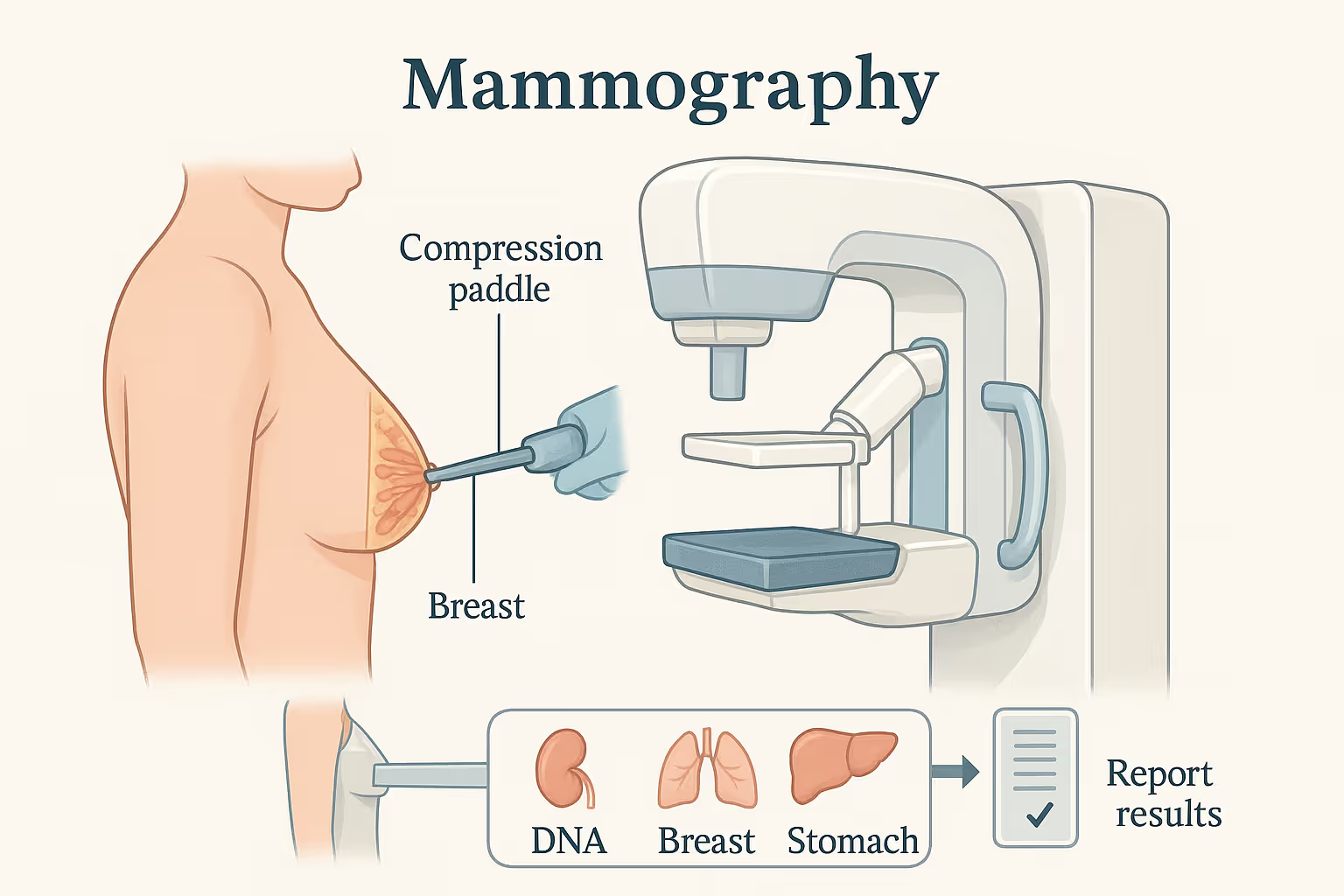
During the procedure, the breast is carefully positioned on a flat support platform, and a compression paddle is gently lowered to evenly spread the breast tissue. This compression is essential for two reasons: it reduces the thickness of the breast, which allows for a lower radiation dose, and it minimizes motion, which helps produce clearer, more accurate images.
Once the breast is compressed, a low-dose X-ray beam passes through the tissue and is captured by a digital detector or film system, depending on the equipment used. These images are then interpreted by a radiologist, an expert in reading medical imaging, to identify any suspicious changes such as masses, calcifications, or architectural distortions.
Advancements such as digital mammography and 3D mammography (also known as digital breast tomosynthesis) provide enhanced image clarity and enable better visualization of dense breast tissue, improving early detection rates.
What is the purpose of mammography?
The primary purpose of mammography is the early detection of breast cancer and other breast-related diseases. By identifying tumors at an earlier stage, when they are typically smaller and more treatable, mammography significantly increases the chances of successful treatment.
Mammograms can reveal changes in breast tissue that may indicate cancer even before physical symptoms appear, serving as both a screening tool for asymptomatic women and a diagnostic tool for those with symptoms. Regular mammography is also used to monitor patients who have a history of breast cancer for any signs of recurrence.
Take a proactive approach to breast health
At Fountain Life, we go beyond standard screenings by integrating cutting-edge diagnostics like 3D mammography with full-body imaging and precision health assessments. Our approach helps detect disease in its earliest stages, before symptoms begin, giving you a better chance at timely, personalized treatment. Whether you’re looking to begin regular screenings or supplement them with more comprehensive insights, our expert team ensures your breast health is never left to chance.
What device is used for mammography?
The device used to perform mammography is called a mammography machine or mammography unit. It is a highly specialized imaging system designed to produce detailed images of the breast using low-dose X-rays. The resulting image is known as a mammogram, abbreviated as MG, and it plays a central role in both breast cancer screening and diagnosis.
A mammography machine consists of several key components. The X-ray tube emits a controlled beam of low-dose radiation. The compression paddles gently press the breast to spread the tissue evenly, which helps reduce motion blur and the amount of radiation needed. Below the breast, a digital detector captures the X-rays that pass through and converts them into high-resolution digital images for evaluation by a radiologist.
Modern mammography machines have advanced significantly, with innovations such as digital mammography, full-field digital mammography (FFDM), and 3D mammography (also called digital breast tomosynthesis). These technologies offer clearer imaging, improved detection of small abnormalities, and better accuracy for women with dense breast tissue. Many systems also integrate computer-aided detection (CAD) to help highlight areas of concern and support radiologists in identifying early signs of breast cancer more effectively.
Can mammograms detect breast cancer?
Yes, mammograms can detect breast cancer by identifying abnormal changes in breast tissue, such as masses, calcifications, or architectural distortions. They are especially effective in spotting cancers at an early stage, often before physical symptoms appear, when treatment is more likely to be successful.
However, while mammography is a powerful screening tool, it is not infallible. Certain factors, such as dense breast tissue, can make it more difficult to detect tumors, potentially leading to false negatives. In such cases, additional imaging methods like breast ultrasound, breast MRI, or 3D mammography may be recommended for further evaluation.
If a mammogram reveals a suspicious area, it does not confirm cancer but rather indicates the need for further testing, such as a biopsy, to determine whether the abnormality is malignant. Despite its limitations, mammography remains the gold standard for routine breast cancer screening due to its ability to detect cancers early and reduce breast cancer mortality.
What is the procedure to perform a mammography?
The mammography procedure is a systematic process that ensures high-quality breast imaging while prioritizing patient comfort and diagnostic accuracy. It involves several essential steps, from initial preparation to final image evaluation. Each step plays a crucial role in detecting breast abnormalities early and ensuring reliable results. Here are the key steps:
- Patient preparation: Patients discuss breast health history, avoid deodorants, and schedule the exam when breasts are least tender.
- Clothing removal: Patients remove clothing from the waist up and wear a gown, removing jewelry to avoid image interference.
- Proper positioning: The technologist positions each breast for standard views to ensure full tissue coverage and image accuracy.
- Breast compression: The breast is gently compressed between two plates to improve image clarity and minimize radiation exposure.
- Image acquisition: Multiple X-ray images are taken using digital or 3D mammography, typically completed in 10–15 minutes.
- Post-imaging procedure: Patients may resume normal activity immediately; a follow-up is advised if further tests are needed.
- Image evaluation and results: A radiologist reviews the images using BI-RADS categories, and results are usually provided within a few days.
Each step is designed to optimize the quality of the images and make the process as efficient as possible. From patient preparation to the final image evaluation, every aspect of the procedure plays a crucial role in detecting breast abnormalities and ensuring the patient’s well-being.
The following sections will provide a detailed overview of each step in the mammography procedure, offering insights into what patients can expect and how each step contributes to a successful mammogram.
1. Patient preparation
Patient preparation is the first and one of the most important steps in ensuring a successful mammogram. This phase involves discussing any current breast concerns or symptoms with a healthcare provider, sharing past mammogram results for comparison, and scheduling the exam during a time when the breasts are least tender, ideally one week after menstruation. Patients are also advised to avoid deodorants, powders, lotions, or perfumes on the day of the exam, as these products can contain metallic particles that may show up on the X-ray and obscure results. Proper preparation helps reduce discomfort during the procedure and improves the accuracy of the images, making it a foundational step in early detection.
2. Clothing removal
Before the imaging process begins, patients are asked to remove all clothing from the waist up and wear a medical gown. Any necklaces or upper-body jewelry must also be removed to prevent interference with the X-ray. Though simple, this step is essential for creating a clear path for imaging and preventing artifacts on the mammogram. Ensuring nothing obstructs the breast area is critical to capturing undistorted, high-resolution images, which are necessary for identifying small abnormalities.
3. Proper positioning
Proper positioning of the breast is crucial for comprehensive imaging. The technologist places the breast in two standard views: the craniocaudal (CC) and the mediolateral oblique (MLO). The CC view captures a top-down image, while the MLO view provides a side-angle that includes the pectoral muscle. These angles are essential to ensure that all areas of the breast tissue, including those near the chest wall, are visualized. Accurate positioning reduces the risk of tissue overlap, motion blur, or missed lesions, directly impacting the reliability of the mammogram.
4. Breast compression
Breast compression is a key technical step that improves image quality and diagnostic accuracy. During compression, the breast is gently but firmly pressed between two flat plates. This spreads the tissue evenly, reduces its thickness, and minimizes motion during the X-ray exposure. The compression lasts only a few seconds per image but significantly enhances clarity while allowing for a lower radiation dose. Although some patients may feel temporary discomfort, this step is vital for detecting small tumors or calcifications that might otherwise be hidden in overlapping tissue.
5. Image acquisition
Image acquisition involves capturing several high-resolution images of each breast using low-dose X-rays. The technologist ensures that images are taken from appropriate angles and that the breast is still and properly compressed. Digital and 3D mammography systems are often used to produce more detailed and layered images. This step typically takes 10 to 15 minutes. High-quality image acquisition is central to identifying subtle abnormalities, and the precision in this phase ensures that follow-up imaging or biopsies are only ordered when truly necessary.
6. Post-imaging procedure
After the mammogram images are taken, patients can change back into their clothes and resume normal activities. They are often advised to wear a supportive bra for the rest of the day to ease any residual tenderness. The radiologist will review the images shortly after the exam, and if any irregularities are observed, patients may be contacted for additional imaging, such as ultrasound or MRI. This step ensures continuity of care and a smooth transition to follow-up if needed, making it an important phase in the patient experience.
7. Image evaluation and results
Image evaluation is conducted by a radiologist who specializes in breast imaging. The radiologist carefully examines the mammogram for signs of masses, asymmetries, or calcifications and categorizes findings using the BI-RADS (Breast Imaging Reporting and Data System) scale. This standardized system helps determine whether the results are normal, benign, suspicious, or require further testing. The accuracy and timeliness of this step are critical to the entire mammography process, as they determine whether additional procedures are necessary. A thorough and expert review ensures early detection of cancer and timely medical intervention when needed.
What are the common issues raised during mammography?
While mammography is a critical tool for early breast cancer detection, several concerns and limitations can arise during the procedure. These issues may affect the accuracy of the results or the patient’s overall experience. Understanding these challenges helps patients better prepare for the exam and allows healthcare providers to take steps to minimize them.
- Discomfort or pain during breast compression
- Increased sensitivity when scheduled near the menstrual cycle
- Difficulty detecting abnormalities in dense breast tissue
- Missed cancers due to improper positioning or poor imaging technique
- Superimposition of overlapping breast and glandular tissue
- Concerns about radiation exposure, especially in pregnant or lactating women
- False-positive results leading to unnecessary stress and follow-up tests

What is the duration of a mammography procedure?
A typical mammography appointment lasts between 20 to 30 minutes. This includes all phases of the procedure, patient preparation, positioning, image acquisition, and post-imaging steps. While the actual compression of each breast only takes about 10 to 15 seconds per image, multiple views are often required to ensure thorough imaging.
Several factors can affect the total duration. These include the patient's ability to remain still, which helps avoid motion blur; the need for additional images if the initial ones are unclear; and the time required for accurate positioning and compression. In some cases, women with dense breast tissue may need extra views or additional imaging, slightly extending the overall appointment time. Despite these variables, the procedure is usually efficient, and patients can return to their regular activities immediately afterward.
When do you have to get a mammogram?
Most women are recommended to begin screening mammograms at age 40, as early detection significantly increases the chances of successful breast cancer treatment. Women aged 40 to 49 should have a personalized discussion with their healthcare provider to decide whether to start annual screenings based on their individual risk factors and preferences.
For women aged 50 to 74, mammograms are generally recommended every one to two years, depending on medical history, breast density, and physician guidance. Regular screening during this period is strongly supported by clinical evidence to reduce breast cancer mortality.
Women aged 75 and older should decide whether to continue mammograms based on their overall health, life expectancy, and discussions with their physician. If a woman is in good health and has a longer life expectancy, continued screening may still be beneficial.
Certain conditions may require earlier or more frequent mammograms. These include having a family history of breast cancer, known genetic mutations like BRCA1 or BRCA2, a personal history of breast cancer, or dense breast tissue. In such cases, mammography may begin before age 40 and be supplemented with other imaging methods like MRI or ultrasound.
Personalized screening plans based on your risk
Fountain Life offers advanced breast cancer screening plans tailored to your unique risk profile, family history, and genetic background. Instead of one-size-fits-all guidelines, we help you determine when to start, how often to screen, and what imaging methods are most effective for your needs. It’s screening on your terms, with precision and confidence.
Can a mammogram detect lung cancer?
No, a mammogram cannot detect lung cancer. Mammography is a diagnostic imaging technique specifically designed to examine breast tissue using low-dose X-rays. It is highly effective for identifying abnormalities such as tumors, cysts, and calcifications within the breast, but it is not capable of visualizing structures in the chest or lungs.
If lung cancer is suspected, other diagnostic tools are required, most commonly a chest X-ray, CT scan, or MRI. These imaging methods are tailored to assess the lungs and surrounding thoracic structures. For accurate screening and early detection of lung cancer, individuals, especially those at high risk, should undergo a dedicated lung cancer screening protocol recommended by their healthcare provider.
Mammograms are also not effective for detecting cancers in other parts of the body, such as ovarian, colon, or pancreatic cancers. Each cancer type typically requires its own specific screening method based on the organ system involved. Therefore, while mammography is essential for breast health, it is not a comprehensive cancer screening tool.
What are the types of mammography?
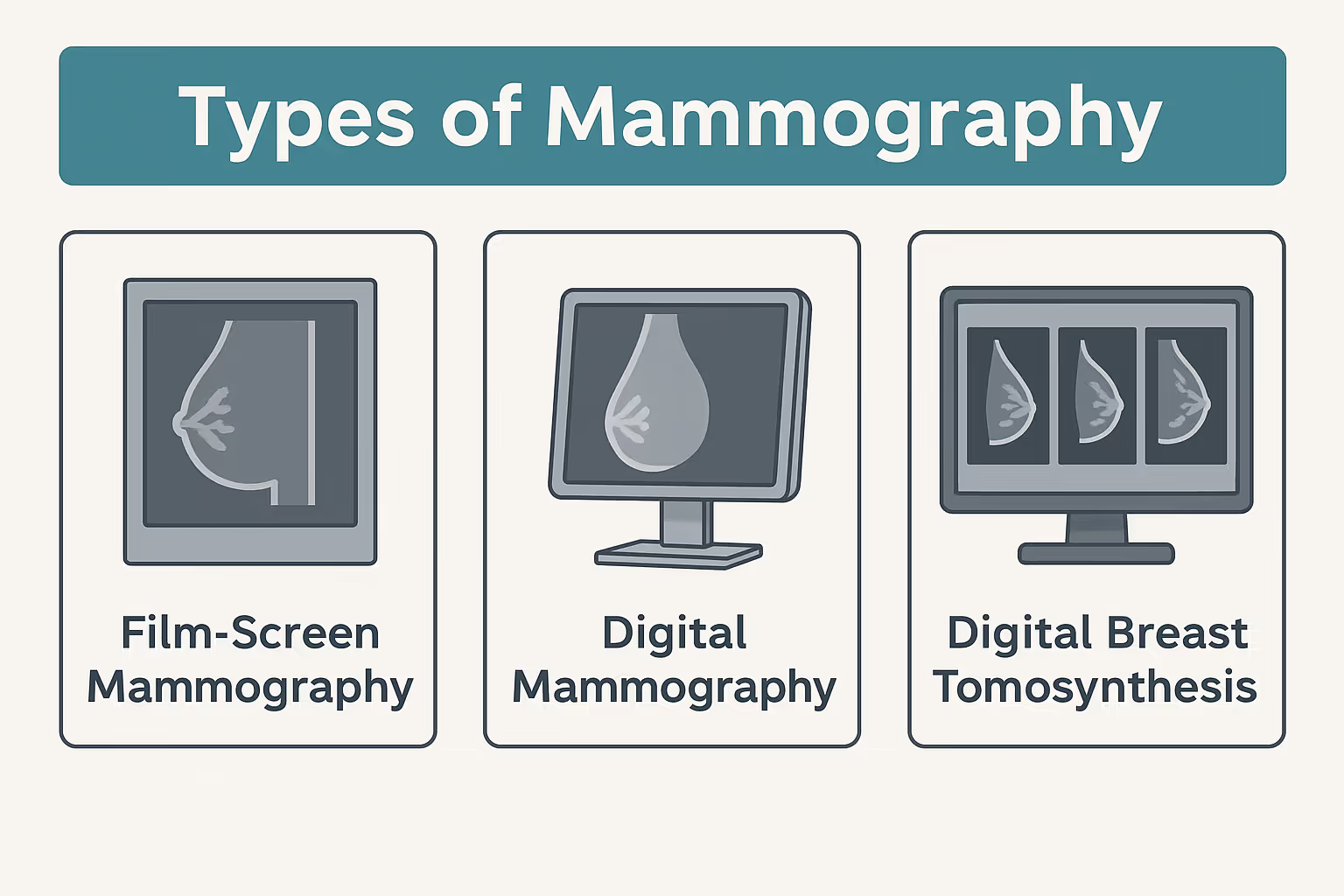
Mammography includes several types of imaging techniques, each designed for a specific purpose in breast health evaluation. These methods vary based on the clinical need, whether routine screening or further investigation, and the technology used to capture breast images.
- Screening mammograms: Used as a routine preventive test for women without symptoms, aiming to detect breast cancer at an early stage.
- Diagnostic mammograms: Performed when symptoms like lumps, pain, or nipple discharge are present, providing more detailed images for evaluation.
- Digital mammography: Uses digital detectors to capture and store electronic breast images, allowing for enhanced viewing, magnification, and sharing.
- 3D mammography (digital breast tomosynthesis): Takes multiple images from different angles to create a layered, three-dimensional view of the breast, improving accuracy, especially in women with dense breast tissue.
Each type plays a critical role in identifying breast abnormalities, with newer technologies offering improved clarity, lower recall rates, and better cancer detection outcomes.
What is the difference between mammography and tomosynthesis?
While both mammography and breast tomosynthesis are used to detect breast abnormalities, they differ in image quality, technique, and diagnostic accuracy. Traditional mammography captures two-dimensional images of the breast, which can sometimes cause overlapping tissue to obscure potential abnormalities. In contrast, tomosynthesis, also known as 3D mammography, takes multiple X-ray images from different angles and reconstructs them into a layered, three-dimensional view, providing greater detail.
Tomosynthesis improves the visibility of tumors, especially in women with dense breast tissue, where conventional mammograms may miss subtle lesions. It also reduces the likelihood of false positives and the need for follow-up imaging, as radiologists can examine each layer of breast tissue separately. Although tomosynthesis involves slightly more radiation than standard mammography, the increased diagnostic accuracy makes it a valuable advancement in breast imaging.