Esophageal cancer screening refers to a group of diagnostic procedures used to detect abnormal or cancerous cells in the esophagus before symptoms develop. While there is no routine or standard screening test recommended for the general population, screening is crucial for individuals at higher risk, such as those with Barrett’s esophagus, long-term acid reflux (GERD), or a family history of esophageal cancer. Early detection can lead to better treatment outcomes, less invasive procedures, and significantly higher survival rates.
This article explores six clinically proven methods used by healthcare professionals to detect esophageal cancer early. You’ll learn what each test involves, how effective it is, who should get screened, and when. If you or someone you know is at risk, understanding these options could make all the difference. Here’s what we’ll cover:
- Esophagoscopy – Visual examination of the esophageal lining using a flexible camera.
- Biopsy – Tissue sampling to confirm or rule out cancer at a cellular level.
- Brush cytology – Cell collection using a soft brush passed through an endoscope.
- Balloon cytology – Retrieval of esophageal cells via a swallowed balloon.
- Chromoendoscopy – Use of contrast dyes to highlight abnormal tissue areas.
- Fluorescence spectroscopy – Light-based imaging that detects early molecular changes.
Read on to learn how each of these screening methods plays a critical role in catching esophageal cancer early, when it's most treatable.
Key Takeaways
- Esophagoscopy is the most effective screening tool for early detection of esophageal cancer, allowing direct visualization and tissue sampling.
- Biopsies and other techniques, like brush cytology and balloon cytology, are essential for accurate diagnosis and assessment of esophageal cancer.
- Several risk factors, including family history, age, and lifestyle choices, influence esophageal cancer screening recommendations for individuals.
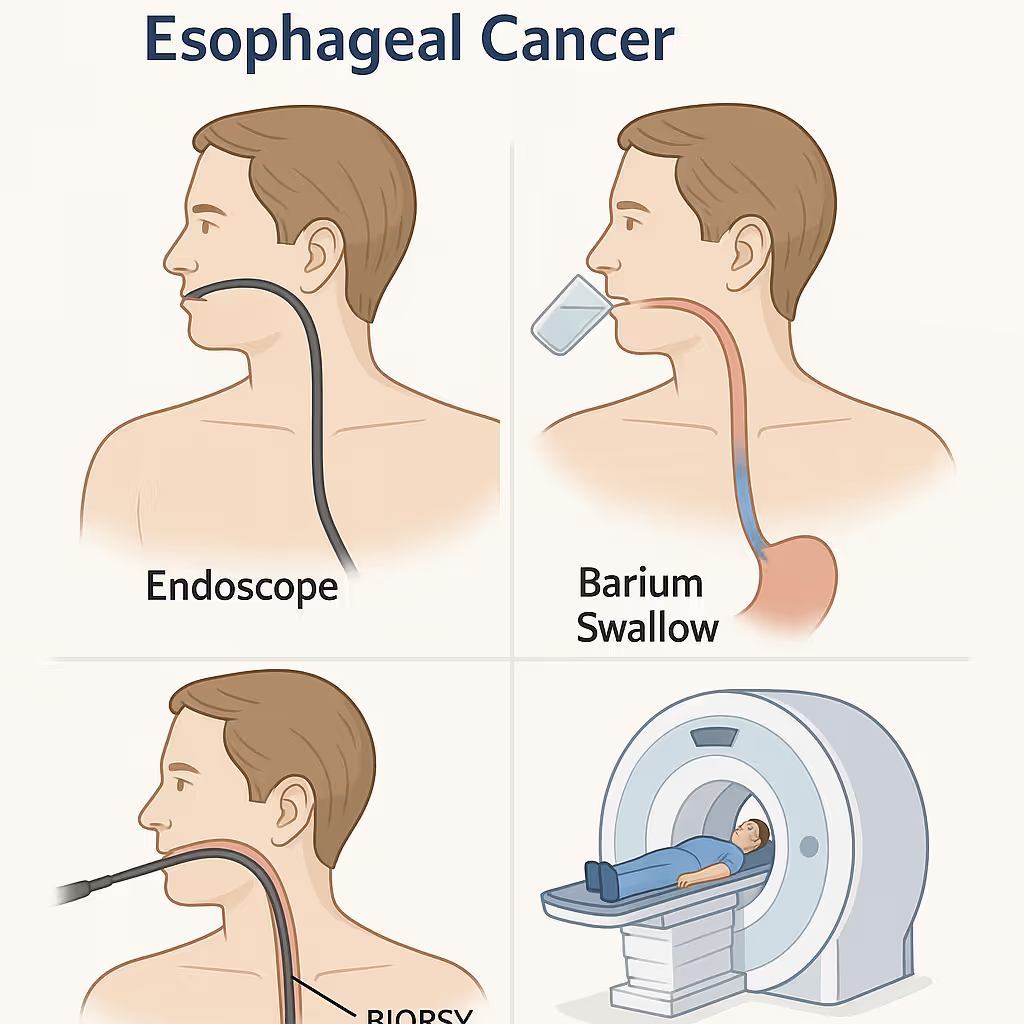
1. Esophagoscopy
Esophagoscopy is a diagnostic procedure used to visually examine the esophagus for early signs of cancer and other abnormalities. It involves inserting a flexible endoscope, a thin tube with a light and camera, through the mouth and down into the esophagus. This allows physicians to inspect the esophageal lining in real time and detect conditions such as Barrett’s esophagus, esophageal squamous cell carcinoma, and early-stage adenocarcinoma.
Esophagoscopy is highly effective for detecting esophageal cancer in its earliest stages. It provides a direct, detailed view of the esophagus, allowing clinicians to identify even small lesions that imaging tests might miss. Its diagnostic accuracy is further enhanced when combined with procedures like endoscopic mucosal resection (EMR), which enables the removal and histological analysis of suspicious tissue during the same procedure.
This test is considered the most important and primary screening method for esophageal cancer, particularly in high-risk individuals. It not only allows for visual diagnosis but also facilitates immediate biopsy or treatment interventions, making it a cornerstone in early detection strategies.
Screening guidelines recommend esophagoscopy for individuals with chronic gastroesophageal reflux disease (GERD), Barrett’s esophagus, or a family history of esophageal cancer. In most cases, screenings begin around age 50, although patients with significant risk factors may need to start earlier based on physician assessment.
The procedure is performed under sedation and typically takes less than 30 minutes. The endoscope is inserted through the mouth and carefully guided down the esophagus to assess the tissue lining. If abnormal areas are found, biopsies or minor procedures can be conducted on the spot.
Screening frequency depends on initial findings and individual risk levels. Patients with confirmed Barrett’s esophagus or prior abnormal results may need annual or biennial follow-ups. For others, a less frequent schedule may be appropriate.
The cost of esophagoscopy varies but is often covered by insurance when deemed medically necessary for high-risk patients. Out-of-pocket costs may depend on the healthcare provider, location, and insurance plan, but the procedure is widely accessible and performed on an outpatient basis.

2. Biopsy
A biopsy is a diagnostic procedure that involves collecting a small tissue sample from the esophagus for microscopic examination. It is often performed alongside an upper endoscopy when visual abnormalities are detected. This technique is essential for confirming the presence of esophageal cancer, providing clear evidence of cancerous or precancerous cells.
Biopsy offers exceptionally high diagnostic accuracy. It enables pathologists to determine whether the sampled tissue contains malignant cells, identify the specific type of esophageal cancer, such as adenocarcinoma or squamous cell carcinoma, and assess the disease’s progression. This information is crucial for developing an individualized and effective treatment plan.
Biopsies are typically recommended when lesions, nodules, or suspicious changes are seen during endoscopic screening. Unlike general screening guidelines, biopsies are not based on age but are instead driven by specific clinical findings. Using specialized instruments passed through the endoscope, physicians collect tissue samples from the affected area, which are then sent to a pathology lab for analysis.
The frequency of biopsies depends on prior screening outcomes and individual risk factors. High-risk individuals, or those with previous abnormal endoscopic findings, may require more frequent biopsies for ongoing evaluation. In cases where initial biopsies are inconclusive, repeat procedures may be necessary to ensure diagnostic clarity.
Biopsy costs can vary depending on the healthcare provider and facility, but the procedure is typically covered by insurance when deemed medically necessary. It is usually performed as part of an outpatient endoscopy, minimizing the need for separate hospital visits.
Biopsies are a critical component of esophageal cancer diagnosis. By delivering definitive pathological insights, they enable early, accurate detection and guide the development of personalized, potentially life-saving treatment strategies.
3. Brush cytology
Brush cytology is a minimally invasive diagnostic technique used to collect surface cells from the esophagus for microscopic analysis. During this procedure, a small brush is passed through an endoscope and gently scraped along the esophageal lining to gather a sample of epithelial cells. These samples are then examined in a laboratory to detect any signs of abnormality.
Brush cytology is effective in identifying early cellular changes associated with esophageal cancer. By collecting a broad range of cells, including those from the stratified squamous epithelium, columnar epithelium, and Barrett’s epithelium, it increases the likelihood of detecting dysplasia, precancerous lesions, or malignancies. Although it is less definitive than a biopsy, brush cytology is valuable for initial screening and monitoring.
This method is frequently used in conjunction with esophagoscopy and is recommended for high-risk individuals. Patients with Barrett’s esophagus, chronic gastroesophageal reflux, or a history of conditions such as oral leukoplakia are often advised to undergo brush cytology. It can be performed at any age if abnormalities are suspected during visual examination or other screening tests.
The procedure involves inserting the brush through an endoscope during an upper endoscopy. The brushing is brief and typically causes minimal discomfort. Collected cells are preserved and sent to a pathology lab for cytological evaluation.
The frequency of brush cytology screenings depends on individual risk profiles and the outcomes of prior tests. High-risk patients may require regular screenings, particularly if previous results have shown atypical cellular changes. The procedure is relatively low-cost and is generally covered by insurance when conducted for medically justified reasons in at-risk populations.
Brush cytology serves as an important screening tool for esophageal cancer, offering a safe, efficient way to detect early-stage cellular abnormalities and support timely clinical intervention.
4. Balloon cytology
Balloon cytology is an innovative, minimally invasive screening method for detecting esophageal cancer. The procedure involves swallowing a deflated balloon attached to a thin catheter. Once the balloon reaches the stomach, it is inflated and gently pulled back through the esophagus, collecting surface cells from the esophageal lining as it moves upward.
This technique is highly effective at collecting a broad spectrum of cells from multiple regions of the esophagus, increasing the likelihood of detecting cancerous or precancerous changes. It is particularly beneficial in identifying early-stage esophageal cancers and conditions such as Barrett’s esophagus, making it a valuable tool in preventive oncology.
Balloon cytology is typically recommended for individuals at elevated risk for esophageal cancer. This includes those with a family history of the disease, persistent gastroesophageal reflux disease (GERD), or related conditions involving the gastric cardia. It can be performed at any age when abnormalities are suspected during preliminary evaluation or when risk factors are present.
The procedure is relatively simple and does not require sedation. The patient swallows the deflated balloon, which is then inflated in the stomach. As it is retracted, the balloon collects cells from the esophageal lining. These cells are then analyzed in a laboratory for signs of dysplasia or malignancy.
Screening frequency varies depending on personal risk factors and previous findings. High-risk patients may undergo annual or biennial balloon cytology to monitor for disease progression. The test is cost-effective compared to other invasive procedures and is often covered by insurance, particularly when performed for individuals with documented risk factors.
Balloon cytology is a valuable screening option for early esophageal cancer detection. Its ability to collect diverse cell samples with minimal discomfort makes it an accessible and efficient choice for high-risk individuals.
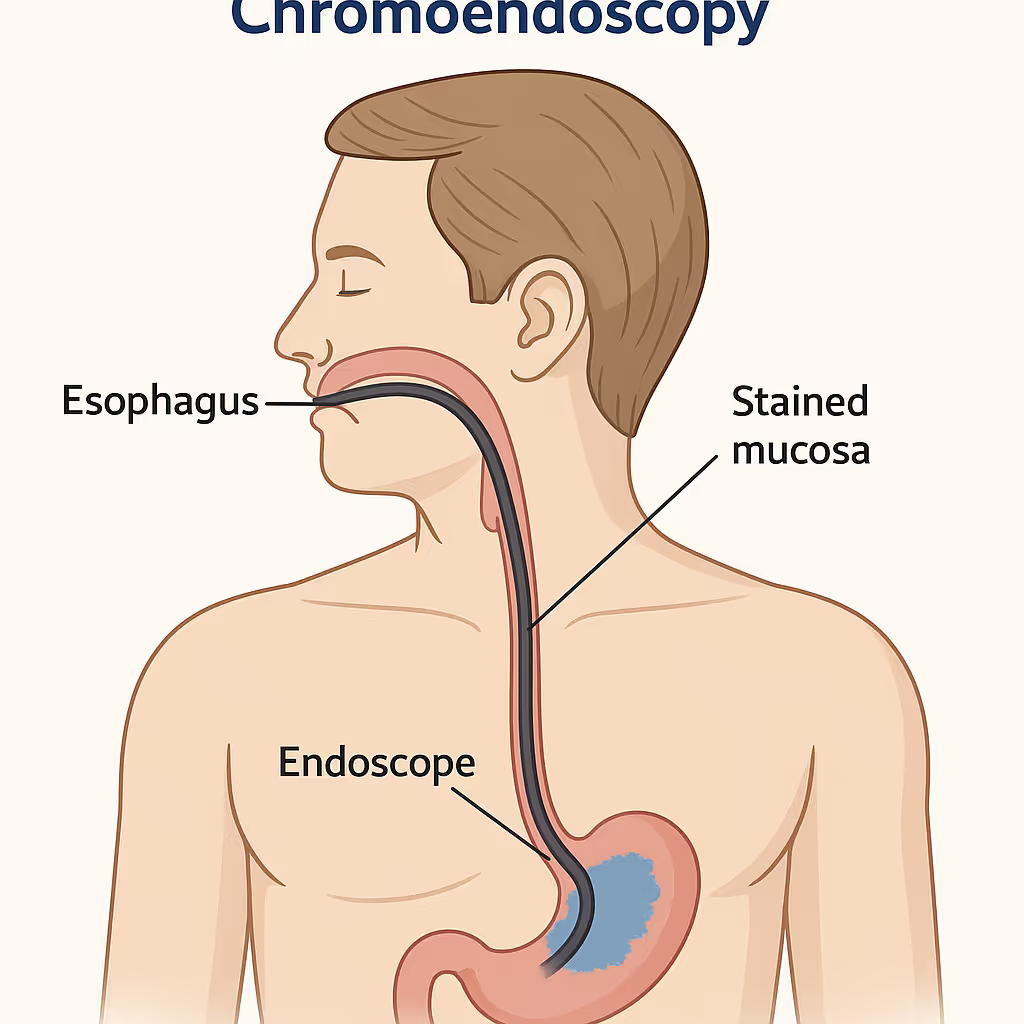
5. Chromoendoscopy
Chromoendoscopy is an advanced endoscopic technique that enhances the visualization of the esophageal lining by applying special dyes or stains during an upper endoscopy. These dyes provide contrast that highlights abnormal or suspicious areas of the mucosa, allowing for a more detailed and accurate examination of the esophagus.
This method is highly effective in increasing the detection rate of early-stage esophageal cancers and precancerous conditions, such as high-grade dysplasia. By accentuating subtle tissue changes that might be missed with standard white-light endoscopy, chromoendoscopy improves diagnostic accuracy and helps guide targeted biopsies.
Chromoendoscopy is most often used in high-risk individuals undergoing gastrointestinal endoscopy or endoscopic ultrasound. It is particularly recommended for patients with Barrett’s esophagus, a history of esophagogastric junction cancers, or persistent GERD symptoms. Screening with this method can begin at any age when significant risk factors are present or when standard endoscopy reveals unclear findings.
The procedure involves the application of contrast dyes, such as Lugol’s iodine or methylene blue, to the esophageal lining through the endoscope. These dyes temporarily stain the mucosa and make abnormal areas more visible for examination or biopsy.
The frequency of chromoendoscopy is determined by a patient’s risk profile and previous screening results. For individuals with confirmed Barrett’s esophagus or prior abnormal findings, regular surveillance may be necessary. The cost is generally higher than standard endoscopy due to the use of specialized dyes and techniques, but it is often covered by insurance when indicated for high-risk cases.
Chromoendoscopy is a powerful tool in the early detection of esophageal cancer. Its enhanced imaging capabilities enable clinicians to identify and assess abnormal tissue changes at a much earlier stage, supporting timely diagnosis and effective treatment planning.
6. Fluorescence spectroscopy
Fluorescence spectroscopy is a cutting-edge diagnostic tool used to detect early esophageal cancer by analyzing tissue fluorescence patterns. During this procedure, a special light is used to excite molecules within the esophageal tissue, causing them to emit fluorescent signals. These signals are then measured and analyzed to identify abnormal cellular or metabolic activity.
This technique is highly effective for detecting early-stage esophageal cancers and precancerous changes. Unlike traditional imaging, fluorescence spectroscopy can reveal metabolic and structural abnormalities at the cellular level, even before visible lesions appear. It is particularly valuable for identifying dysplasia in patients with Barrett’s esophagus or chronic gastroesophageal reflux.
Fluorescence spectroscopy is typically performed in conjunction with an upper endoscopy. It is recommended for individuals at high risk for esophageal cancer, including those with a history of GERD, Barrett’s esophagus, or a family history of upper gastrointestinal malignancies. Screening can begin at any age when significant risk factors are identified by a healthcare provider.
The procedure involves inserting a specialized probe through the endoscope during endoscopy. This probe emits and measures light-induced fluorescence in the esophageal lining, allowing clinicians to detect subtle changes in tissue composition and function. It is non-destructive and adds minimal time to a standard endoscopic exam.
Screening frequency depends on the patient’s risk level and previous findings. Individuals with ongoing symptoms or a history of abnormal screenings may require periodic monitoring. Due to the use of advanced imaging technology, the cost of fluorescence spectroscopy is typically higher than conventional endoscopy, but is often covered by insurance when medically indicated for high-risk patients.
Fluorescence spectroscopy is an advanced and valuable screening method for esophageal cancer. Its ability to detect changes at the molecular level makes it a promising tool for identifying early cancerous transformations and guiding timely clinical intervention.
What is the best way to detect Esophageal Cancer early?
The most effective method for the early detection of esophageal cancer is esophagoscopy. It is widely regarded as the gold standard because it offers both direct visualization of the esophageal lining and the ability to collect tissue samples through biopsy. This dual function allows clinicians to identify even the smallest precancerous or cancerous lesions and immediately investigate them further, leading to a highly accurate diagnosis.
Unlike cancer screening tests that rely solely on imaging or lab analysis, esophagoscopy provides real-time, high-resolution views of the mucosa. When combined with procedures like endoscopic mucosal resection, it also enables immediate removal of abnormal areas for histological evaluation. This comprehensive diagnostic capability not only improves the likelihood of detecting esophageal cancer at an early and treatable stage but also allows for faster, targeted intervention, making it the most reliable screening method available.
Personalized early cancer detection with Fountain Life
At Fountain Life, early detection isn’t just a service, it’s a priority. Through advanced diagnostics and precision screening, Fountain Life helps individuals identify esophageal and other cancers before symptoms appear. Using tools like high-resolution endoscopy, endoscopic biopsy, and molecular imaging, their approach ensures abnormalities are caught at the earliest, most treatable stages.
If you're in a high-risk group or want to take a proactive approach to your health, Fountain Life’s comprehensive cancer screening programs are designed to deliver clarity and peace of mind. Their clinically advanced technologies go beyond conventional checkups, empowering you to take control of your long-term health trajectory.
Can you test for esophageal cancer at home?
No, esophageal cancer cannot be accurately tested for at home. The screening and diagnosis of this cancer require advanced medical procedures, such as esophagoscopy, biopsy, and cytology, that can only be performed by trained professionals in a clinical environment. These tests involve inserting specialized instruments into the esophagus, visually inspecting the lining, and collecting tissue or cell samples for laboratory analysis. This level of precision and accuracy is not achievable with any current home testing kit.
Although home-based tests exist for certain cancers like colorectal or cervical cancer, the anatomy and complexity of the esophagus make at-home sampling impractical and unreliable. Detecting esophageal cancer also depends on visualizing subtle lesions or microscopic cellular changes that require high-resolution imaging and pathologic expertise.
For these reasons, authoritative organizations like the American Cancer Society and the National Cancer Institute recommend that individuals at risk, such as those with GERD, Barrett’s esophagus, or a family history of gastrointestinal cancers, undergo regular screenings in a healthcare setting. Early clinical detection significantly improves treatment success and long-term outcomes.
Can Esophageal Cancer be screened using X-rays?
No, X-rays are not recommended for screening esophageal cancer. While they may detect large, advanced tumors, X-rays lack the sensitivity and resolution needed to identify early-stage cancers or precancerous changes. Most early lesions in the esophagus are flat or subtle and do not produce visible abnormalities on standard X-ray images.
The main limitation of X-rays lies in their inability to provide detailed views of the esophageal mucosa. Unlike more advanced techniques such as esophagoscopy or chromoendoscopy, X-rays cannot visualize minor tissue changes or facilitate biopsy, which are essential for accurate diagnosis. Even with a barium swallow study, a contrast-enhanced x-ray often used to assess swallowing disorders, the detection of early cancer remains unreliable.
For effective screening, medical guidelines recommend direct visualization and tissue sampling through endoscopic procedures, which offer significantly greater diagnostic accuracy. Therefore, X-rays are not considered an appropriate or effective tool for early esophageal cancer detection.
Can a CT scan detect esophageal cancer?
Yes, CT scans can detect esophageal cancer, but they are primarily used to assess the extent and spread of the disease rather than for initial screening. CT scans provide detailed cross-sectional images of the body, which can help identify tumors and determine if cancer has spread to other organs or lymph nodes.
While CT scans are useful for staging esophageal cancer, they are not the most effective tool for early detection. They might miss small or early-stage tumors that can be identified through more specialized procedures like esophagoscopy or biopsy. However, once esophageal cancer is suspected or diagnosed, CT scans play a crucial role in planning treatment and monitoring the disease’s progression.
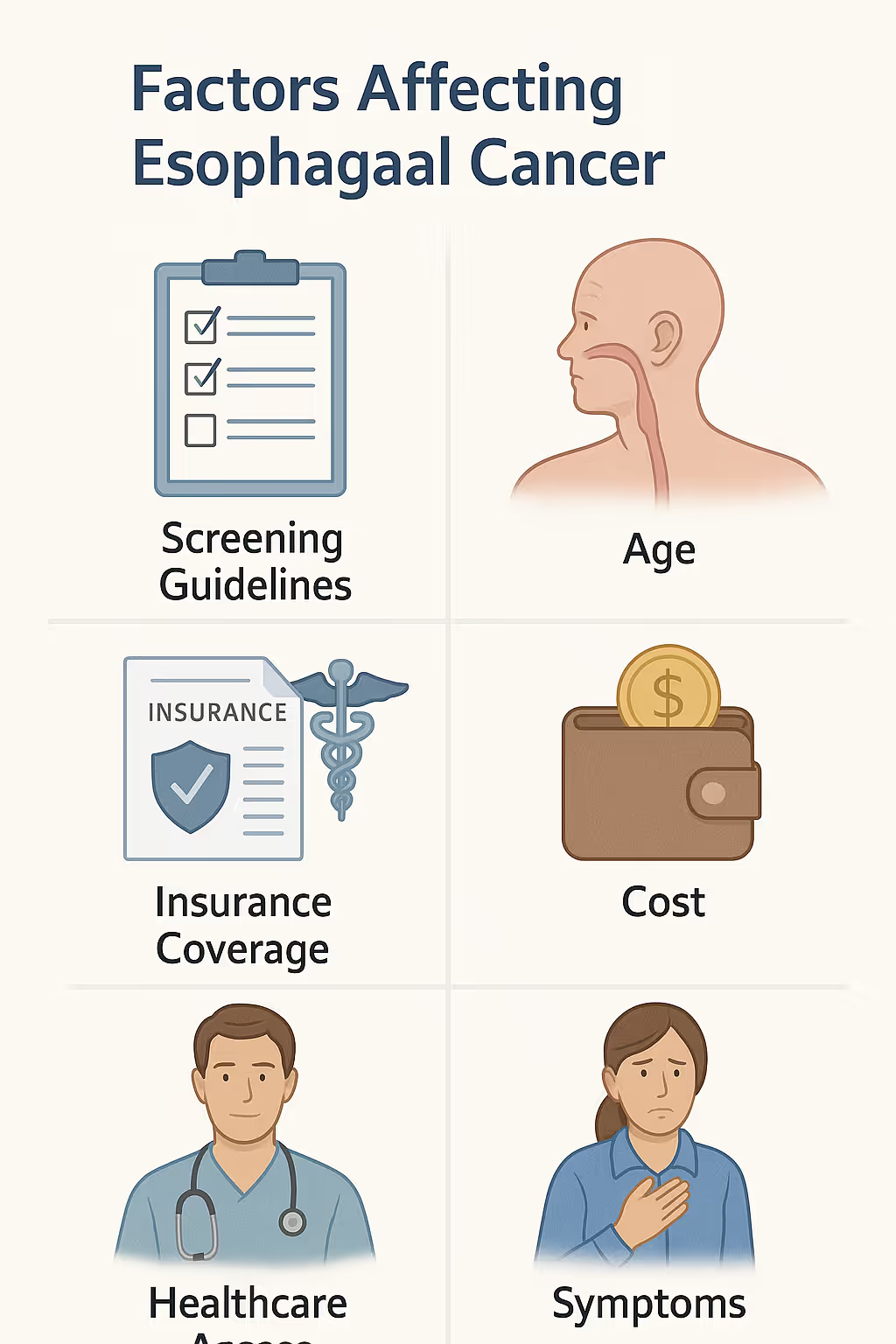
What Factors Affect Esophageal Cancer Screening?
Several factors influence when and how often an individual should be screened for esophageal cancer. These factors help determine risk levels and guide personalized screening protocols.
- Family history: A strong family history of esophageal cancer significantly increases risk. Individuals with first-degree relatives affected by the disease are more likely to develop it themselves and may require earlier and more frequent screenings.
- Age: The likelihood of esophageal cancer increases with age, especially after 50. Most screening guidelines recommend starting around this age for at-risk individuals.
- Gender: Men are more likely to develop esophageal cancer than women, particularly esophageal adenocarcinoma. This gender disparity informs screening strategies.
- Barrett’s esophagus: This condition, where the esophageal lining changes due to chronic acid exposure, is a known precursor to esophageal adenocarcinoma. Regular surveillance is recommended.
- Gastroesophageal reflux disease (GERD): Chronic GERD can lead to Barrett’s esophagus and esophageal inflammation, both of which raise cancer risk. Long-standing GERD symptoms often warrant further evaluation.
- Obesity: Obesity is linked to increased abdominal pressure and chronic reflux, raising the risk of Barrett’s esophagus and esophageal cancer.
- Smoking: Tobacco use significantly increases the risk of esophageal squamous cell carcinoma. It also exacerbates the effects of other risk factors.
- Alcohol consumption: Heavy alcohol intake is strongly associated with squamous cell carcinoma of the esophagus, especially when combined with smoking.
- Diet low in fruits and vegetables: Poor dietary habits may reduce the intake of protective antioxidants and vitamins, modestly increasing esophageal cancer risk.
- Ethnicity and geography: Certain regions and ethnic groups show higher prevalence of specific esophageal cancer subtypes, affecting screening strategies in those populations.
By accounting for these factors, healthcare providers can tailor screening schedules to individual risk profiles, improving the likelihood of early detection and more effective treatment.
What are the benefits of detecting esophageal cancer early?
Detecting esophageal cancer in its early stages provides numerous medical and quality-of-life advantages. Early identification improves prognosis and allows for less aggressive, more effective treatment. Key benefits include:
- Higher survival rates: Early-stage esophageal cancer has a significantly better prognosis, with five-year survival rates reaching up to 47% when diagnosed before metastasis.
- Less invasive treatment options: Early detection often enables the use of minimally invasive procedures such as endoscopic mucosal resection instead of major surgery or chemotherapy.
- Greater chance of curative treatment: When caught early, esophageal cancer is more likely to be treated completely, reducing the need for long-term therapies.
- Lower treatment costs: Managing cancer at an early stage is typically less expensive than treating advanced disease, which may require surgery, radiation, and prolonged hospitalization.
- Reduced treatment side effects: Early-stage treatments tend to have fewer side effects, preserving patient quality of life and reducing complications.
- Improved quality of life: Patients diagnosed early are more likely to maintain normal swallowing, nutrition, and overall health without significant disruption.
- Increased eligibility for clinical trials: Some investigational therapies are only available to patients with early-stage cancer, offering access to advanced care options.
By emphasizing early detection of cancer, patients and healthcare providers can intervene before the disease progresses, significantly improving long-term outcomes.
Take control of your health with proactive screening
Fountain Life offers state-of-the-art screening solutions tailored to your unique risk profile. Whether you have a family history of esophageal cancer, chronic reflux, or simply want a comprehensive overview of your internal health, their preventive screening model enables earlier detection and timely intervention, well before symptoms emerge.
With access to leading-edge diagnostics and a team of medical experts focused on longevity and disease prevention, Fountain Life provides the support you need to stay ahead of serious conditions like esophageal cancer. It’s not just about extending lifeit’s about enhancing the quality of it.