Colorectal cancer screening refers to a group of preventive tests used to detect cancer or precancerous polyps in the colon and rectum before symptoms appear. These screenings are critical for identifying early-stage disease, enabling timely treatment, and preventing cancer from developing.
Several screening methods are available, including colonoscopy, stool-based tests like FIT and DNA stool tests, flexible sigmoidoscopy, and virtual colonoscopy. Each method varies in accuracy, frequency, and level of invasiveness, with colonoscopy being the most comprehensive and widely recommended.
Current guidelines recommend that individuals at average risk begin colorectal cancer screening at age 45. The frequency and type of test depend on personal risk factors and should be determined in consultation with a healthcare provider.
The cost of screening varies by method, ranging from approximately $24 for stool tests to over $600 for a colonoscopy. Most insurance plans, including Medicare, typically cover these tests as part of preventive care.
Key Takeaways
- Colorectal cancer screening is essential for early detection of cancerous growths and precursors in asymptomatic individuals, significantly increasing treatment success rates.
- Screening guidelines recommend starting at age 45 for average-risk individuals, with specific intervals for different tests, facilitating timely intervention and prevention.
- Colonoscopy is the gold standard for colorectal cancer screening due to its high sensitivity and ability to both detect and remove polyps, while various other non-invasive methods exist for individuals with different preferences.
What is Colorectal Cancer Screening?
Colorectal cancer screening refers to a series of medical tests used to detect signs of cancer or precancerous growths in the colon and rectum before symptoms appear. These tests are designed for individuals without symptoms, with the primary goal of identifying colorectal cancer at an early, more treatable stage, or even preventing it altogether by detecting and removing abnormal growths called polyps.
Screening plays a crucial role in reducing the incidence and mortality of colorectal cancer. By identifying cancer in its earliest stages or finding polyps before they become cancerous, screening significantly improves treatment outcomes and long-term survival.
There are several screening methods available, ranging from visual exams like colonoscopy and sigmoidoscopy to non-invasive stool-based tests such as the fecal immunochemical test (FIT) and stool DNA tests. Each method has specific advantages, limitations, and recommended intervals based on an individual's age and risk factors.
Leading health organizations, including the American Cancer Society, recommend routine colorectal cancer screening starting at age 45 for individuals at average risk. For those with a family history or other risk factors, screening may need to begin earlier and be performed more frequently.
Understanding your screening options and consulting a healthcare provider ensures you choose the most appropriate test for your needs. The following sections will break down how these tests work, their frequency, and which method might be best suited for different individuals.
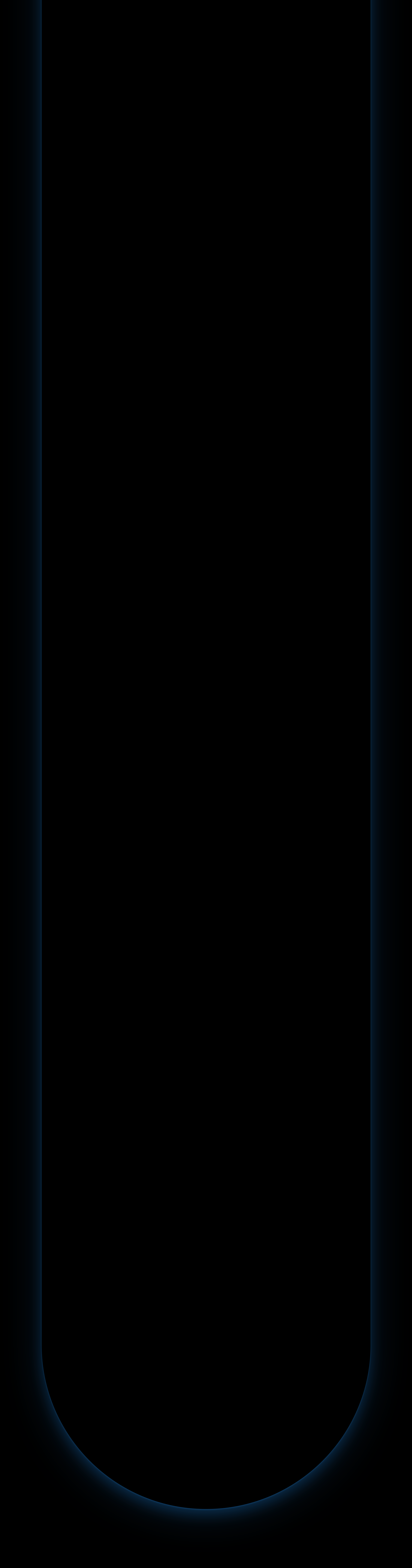
How does Colorectal Cancer Screening work
Colorectal cancer screening works by detecting abnormal growths, such as precancerous polyps or early-stage cancers, in the colon or rectum before any symptoms appear. These tests are used as a preventive tool, aiming to catch potential issues early when treatment is most effective and the chances of a full recovery are highest.
Unlike diagnostic tests, which are used when symptoms are already present, screening tests are performed on asymptomatic individuals. Their primary goal is to identify small polyps or early signs of cancer that can be removed or treated before they progress into advanced disease. Each screening method works differently:
- Stool-based tests look for hidden blood or abnormal DNA in a stool sample, which can signal the presence of polyps or cancer.
- Visual exams, like colonoscopy or CT colonography, allow direct or image-based inspection of the colon to detect and sometimes remove abnormalities.
If a non-invasive screening test yields a positive result, a follow-up procedure, usually a colonoscopy, is recommended to confirm the findings and, if necessary, remove any polyps.
Most individuals at average risk should begin colorectal cancer screening at age 45. Those with higher risk factors, such as a personal or family history of colorectal cancer or inflammatory bowel disease, may need to begin earlier and screen more frequently.
Regular screening plays a key role in reducing colorectal cancer incidence and mortality by ensuring early detection and timely intervention.
Optimize your screening strategy with Fountain Life
At Fountain Life, we specialize in proactive, precision-based health assessments that go beyond standard screenings. Our advanced diagnostics include high-resolution imaging and genomic testing, enabling earlier detection of cancers, often before symptoms or traditional tests would detect them. If you're considering colorectal cancer screening, Fountain Life provides personalized plans that incorporate your unique risk profile to identify the best course of action for prevention and long-term health.
How to screen for colorectal cancer?
Colorectal cancer screening can be performed using several methods, each designed to detect early signs of cancer or precancerous polyps in individuals without symptoms. For most people, screening begins at age 45, but those with higher risk factors, such as a family history of colorectal cancer, may need to start earlier. The choice of screening method depends on medical history, risk level, and personal preference. Below are the primary colorectal cancer screening methods:
- Fecal occult blood test (FOBT): A stool-based test that detects hidden (occult) blood in the stool, which may indicate bleeding from polyps or cancer. It typically requires dietary restrictions and is performed annually.
- Fecal immunochemical test (FIT): A modern stool test that uses antibodies to detect human blood in the stool. It is more specific than FOBT and does not require dietary restrictions. FIT is also performed annually.
- Stool DNA test (e.g., Cologuard): This test detects both hidden blood and DNA mutations linked to colorectal cancer in stool samples. It is non-invasive and recommended every one to three years, depending on the test type.
- Flexible sigmoidoscopy: A visual exam that uses a flexible, lighted tube to inspect the lower part of the colon and rectum. It is typically performed every five years or every ten years if combined with annual FIT.
- Colonoscopy: Considered the gold standard, this test uses a flexible tube with a camera to examine the entire colon. It allows for the detection and removal of polyps during the same procedure and is usually recommended every ten years.
- Virtual colonoscopy (CT colonography): A less invasive imaging test that uses CT scans to create detailed images of the colon and rectum. It is typically recommended every five years and may require a follow-up colonoscopy if abnormalities are found.
Each of these methods has its own benefits, accuracy levels, and follow-up requirements. Consulting a healthcare provider is essential to choose the most appropriate screening strategy for your individual risk profile.
1. Fecal occult blood test (FOBT)
The fecal occult blood test (FOBT) is a non-invasive stool-based screening method that detects hidden (occult) blood in the stool, which may be a sign of colorectal cancer or large polyps. It is one of the oldest screening methods and typically requires multiple stool samples collected over several days.
FOBT is moderately effective in detecting colorectal cancer. Its sensitivity is lower than more modern tests like FIT or colonoscopy, particularly for detecting polyps or early-stage cancers. However, it remains a valuable tool in settings where more advanced tests are not available.
FOBT is not considered the primary or most accurate test for colorectal cancer screening, but it can be used as an accessible and affordable option, especially when combined with other screening tools.
According to U.S. guidelines, FOBT should be performed annually, starting at age 45 for average-risk individuals. Those with higher risk factors may need to begin screening earlier and with more sensitive methods.
To perform the test, the individual collects small stool samples at home using a provided kit. The samples are then analyzed in a laboratory for traces of blood. Dietary restrictions are often necessary before testing to avoid false positives.
The cost of FOBT is relatively low, averaging around $5–$20, and it is typically covered by insurance as part of preventive care.
2. Fecal immunochemical test (FIT)
The fecal immunochemical test (FIT) is a stool-based screening method that uses antibodies to detect hidden human blood in the lower digestive tract. It offers higher specificity and fewer false positives than FOBT, making it a more accurate tool for colorectal cancer screening.
FIT is effective for detecting early-stage colorectal cancer and large polyps. It has better sensitivity than traditional FOBT and does not require dietary restrictions, which improves patient compliance.
Although not the most comprehensive test, FIT is an important screening method, especially for individuals seeking a non-invasive and cost-effective option. It is often used as a first-line test for average-risk individuals and followed by a colonoscopy if results are positive.
Guidelines recommend annual FIT testing starting at age 45 for those at average risk. People with increased risk factors may require earlier or more frequent screening.
FIT is performed by collecting a single stool sample at home using a special test kit. The sample is then mailed or brought to a lab for analysis.
The average cost of a FIT test is around $24. It is generally covered by insurance and included in preventive care services.
3. Stool DNA test (e.g., Cologuard)
The stool DNA test, such as Cologuard, is a non-invasive screening tool that combines FIT with genetic testing to detect abnormal DNA and hidden blood in stool samples. It is designed to identify DNA mutations associated with colorectal cancer and precancerous polyps.
Stool DNA tests are highly effective, with a sensitivity of over 90% for colorectal cancer and about 40% for large precancerous polyps. However, false positives can occur, and follow-up with a colonoscopy is necessary if results are abnormal.
While not the primary screening method, stool DNA tests are a strong alternative for patients who prefer to avoid invasive procedures. They are especially useful for those at average risk who are unwilling or unable to undergo a colonoscopy.
Screening guidelines recommend stool DNA testing every 1 to 3 years starting at age 45 for average-risk individuals. The frequency may vary based on individual health profiles and physician recommendations.
The process involves collecting an entire bowel movement at home using a provided kit and sending the sample to a lab for analysis.
Cologuard costs around $121, and many insurance plans cover it as part of preventive screening. However, patients should confirm with their provider.
4. Flexible sigmoidoscopy
Flexible sigmoidoscopy is a visual screening method that uses a flexible, lighted tube with a camera to examine the rectum and lower part of the colon (sigmoid colon) for abnormal growths or signs of cancer. It is less invasive than a full colonoscopy, but only evaluates part of the colon.
This test is moderately effective, especially for detecting cancers and polyps in the distal colon. However, it may miss abnormalities in the upper colon, limiting its diagnostic reach compared to colonoscopy.
Flexible sigmoidoscopy is not the primary screening tool, but may be recommended in combination with stool-based tests like FIT for broader coverage. It is a good option for those who cannot undergo a full colonoscopy.
The U.S. Preventive Services Task Force recommends flexible sigmoidoscopy every five years or every ten years if combined with annual FIT, starting at age 45.
To perform the test, a healthcare provider inserts a flexible tube into the rectum to visually inspect the lower colon. Bowel preparation is required, but it is less extensive than that required for colonoscopy.
The average cost ranges from $200 to $500, and it is typically covered by insurance as a preventive screening procedure.
5. Colonoscopy
Colonoscopy is the most comprehensive colorectal cancer screening method. It allows direct visualization of the entire colon and rectum using a flexible tube with a camera and enables the removal of polyps or tissue samples during the same procedure.
Colonoscopy is the most accurate and effective test for detecting both early-stage colorectal cancer and precancerous polyps. It is the only method that is both diagnostic and therapeutic in a single session.
Colonoscopy is considered the gold standard for colorectal cancer screening. It is the primary method recommended by most medical organizations due to its high sensitivity, broad coverage, and ability to prevent cancer by removing polyps during the exam.
Screening guidelines recommend a colonoscopy every ten years starting at age 45 for average-risk individuals. Higher-risk individuals may need earlier or more frequent screening.
The procedure requires a full bowel cleanse with laxatives the day before. It is usually performed under sedation and takes about 30 minutes. Afterward, patients need time to recover from sedation and may require assistance getting home.
The average cost of a colonoscopy is approximately $635. While the procedure is often covered by insurance, patients may incur additional charges if polyps are removed or biopsies are taken.
6. Virtual colonoscopy (CT colonography)
Virtual colonoscopy, or CT colonography, is a minimally invasive imaging test that uses low-dose computed tomography (CT) scans to create detailed images of the colon and rectum. It is an alternative for individuals who cannot or prefer not to undergo a traditional colonoscopy.
Virtual colonoscopy is fairly accurate for detecting larger polyps and colorectal cancers. However, it is less effective for identifying small or flat lesions and cannot remove polyps if found, requiring a follow-up colonoscopy for treatment.
Although not the most important screening method, CT colonography is a reasonable alternative for those seeking a less invasive option. It is often recommended when a colonoscopy is incomplete or not tolerated.
Screening guidelines suggest CT colonography every five years starting at age 45 for average-risk individuals. It is not typically recommended for high-risk patients as a standalone method.
The test involves a bowel cleanse, insertion of a small tube into the rectum to inflate the colon with air, and a CT scan while the patient lies on the scanning table.
The average cost ranges from $400 to $800, depending on location and provider. Insurance coverage varies, so it is essential to check with your health plan.
Can a blood test be used to detect colorectal cancer?
No, a blood test is not currently a reliable or recommended method for colorectal cancer screening. While blood tests are being studied for their potential to detect cancer-specific biomarkers, they are not accurate enough at this time to replace established screening methods like colonoscopy or stool-based tests. Current research focuses on identifying tumor markers such as carcinoembryonic antigen (CEA) and circulating tumor DNA (ctDNA), but these markers lack the sensitivity and specificity required for early detection in asymptomatic individuals.
Blood tests may help monitor treatment response or cancer recurrence in diagnosed patients, but they are not effective as a standalone tool for detecting early-stage colorectal cancer or precancerous polyps.
What is the best Colorectal Cancer Screening test?
The best colorectal cancer screening test is a colonoscopy. Colonoscopy is considered the gold standard because it offers both detection and treatment in a single procedure. Unlike other methods, it allows for direct visualization of the entire colon and rectum, enabling physicians to identify and remove precancerous polyps immediately, preventing them from developing into cancer.
Its diagnostic accuracy is unmatched, with a high sensitivity for detecting both early-stage cancers and small or flat polyps that may be missed by other tests. This level of precision significantly reduces colorectal cancer incidence and mortality when performed at recommended intervals.
While non-invasive alternatives like the fecal immunochemical test (FIT) or stool DNA tests offer convenience, they lack the ability to treat during screening and often require a follow-up colonoscopy if abnormalities are found. Therefore, colonoscopy stands out as the most comprehensive and effective option for both prevention and early detection.
For individuals at average risk, screening with colonoscopy is typically recommended every ten years starting at age 45. Its ability to prevent cancer, not just detect it, is what makes it the most valuable tool in colorectal cancer screening today.
What are the guidelines for screening for colorectal cancer?
Colorectal cancer screening guidelines provide evidence-based recommendations on when individuals should begin screening, how frequently each test should be performed, and which methods are appropriate based on age and risk level. These guidelines are established by leading health authorities to promote early detection, improve survival rates, and reduce cancer incidence. Below are the key colorectal cancer screening guidelines:
- Screening should begin at age 45 for individuals at average risk.
- Those with higher risk factors, such as a family history of colorectal cancer, genetic syndromes, or inflammatory bowel disease, should start earlier and may need more frequent testing.
- Fecal immunochemical test (FIT) and guaiac-based fecal occult blood test (gFOBT) should be done every year.
- Stool DNA test (e.g., Cologuard) is recommended every 1 to 3 years, depending on individual risk.
- Colonoscopy is recommended every 10 years if no abnormalities are found.
- Flexible sigmoidoscopy should be performed every 5 years, or every 10 years if combined with annual FIT.
- CT colonography (virtual colonoscopy) is suggested every 5 years.
- Individuals aged 76 to 85 should discuss screening needs with their healthcare provider, considering overall health and prior screening history.
- Screening is generally not recommended after age 85, unless clinically justified.
Following these guidelines helps ensure the timely detection of colorectal cancer or precancerous polyps, ultimately improving treatment outcomes and reducing healthcare burdens.

What is the cost of a colorectal cancer screening test?
The cost of colorectal cancer screening tests varies depending on the type of test. The average cost for a fecal immunochemical test (FIT) is approximately $24, while a Cologuard test costs around $121. Colonoscopy, being more comprehensive, is more expensive, with an estimated cost of around $635. However, it is often covered by most insurance plans without additional fees for related services.
Patients using non-invasive tests like FIT or Cologuard may need to follow up with a colonoscopy if results are positive, adding potential costs. Despite the initial expense, increasing screening rates to 80% could significantly lower the number of new colorectal cancer cases and associated treatment costs.
The economic burden of colorectal cancer care highlights the importance of early detection and preventive measures.
Fountain Life: Early detection without compromise
While cost can be a barrier to comprehensive preventive care, Fountain Life is committed to making early detection more accessible. Through our membership-based model, clients gain access to cutting-edge screening technologies, including full-body MRI, advanced blood biomarkers, and AI-assisted colon screening tools, all bundled under one proactive health plan. It’s an investment in longevity that eliminates uncertainty and delivers clarity about your long-term wellness.
Is colorectal cancer screening covered by insurance?
Yes, colorectal cancer screening is typically covered by insurance. Most health insurance plans, including Medicare, cover the cost of colorectal cancer screening tests as part of preventive care services. The Affordable Care Act mandates that insurance plans cover preventive services, including colorectal cancer screening, without charging a copayment or coinsurance if the services are provided by an in-network provider.
Insurance coverage generally includes various screening tests such as colonoscopy, fecal immunochemical test (FIT), and stool DNA tests. However, checking with your specific insurance provider is necessary to understand the details of your coverage and any potential out-of-pocket costs.
Coverage for follow-up procedures, such as a colonoscopy after a positive stool test, is also typically included, ensuring that comprehensive care is accessible and affordable for those undergoing screening.
How often should you perform Colorectal Cancer Screening?
The frequency of colorectal cancer screening varies based on the type of test used and an individual's risk level. For average-risk adults, screening typically begins at age 45 and continues through age 75. After age 75, screening decisions should be personalized based on overall health and previous screening history. Individuals with higher risk factors, such as a family history or genetic predisposition, may require earlier and more frequent testing. Below is the recommended screening frequency for each method:
- Fecal immunochemical test (FIT): once every year
- Guaiac-based fecal occult blood test (gFOBT): once every year
- Stool DNA test (e.g., Cologuard): once every 1 to 3 years, depending on individual health status
- Colonoscopy: once every 10 years
- Flexible sigmoidoscopy: once every 5 years, or every 10 years if combined with annual FIT
- CT colonography (virtual colonoscopy): once every 5 years
These timeframes ensure timely detection of colorectal cancer and precancerous polyps, enhancing the chances of early treatment and prevention. Regular screening is essential for maintaining long-term colorectal health and reducing cancer-related mortality.
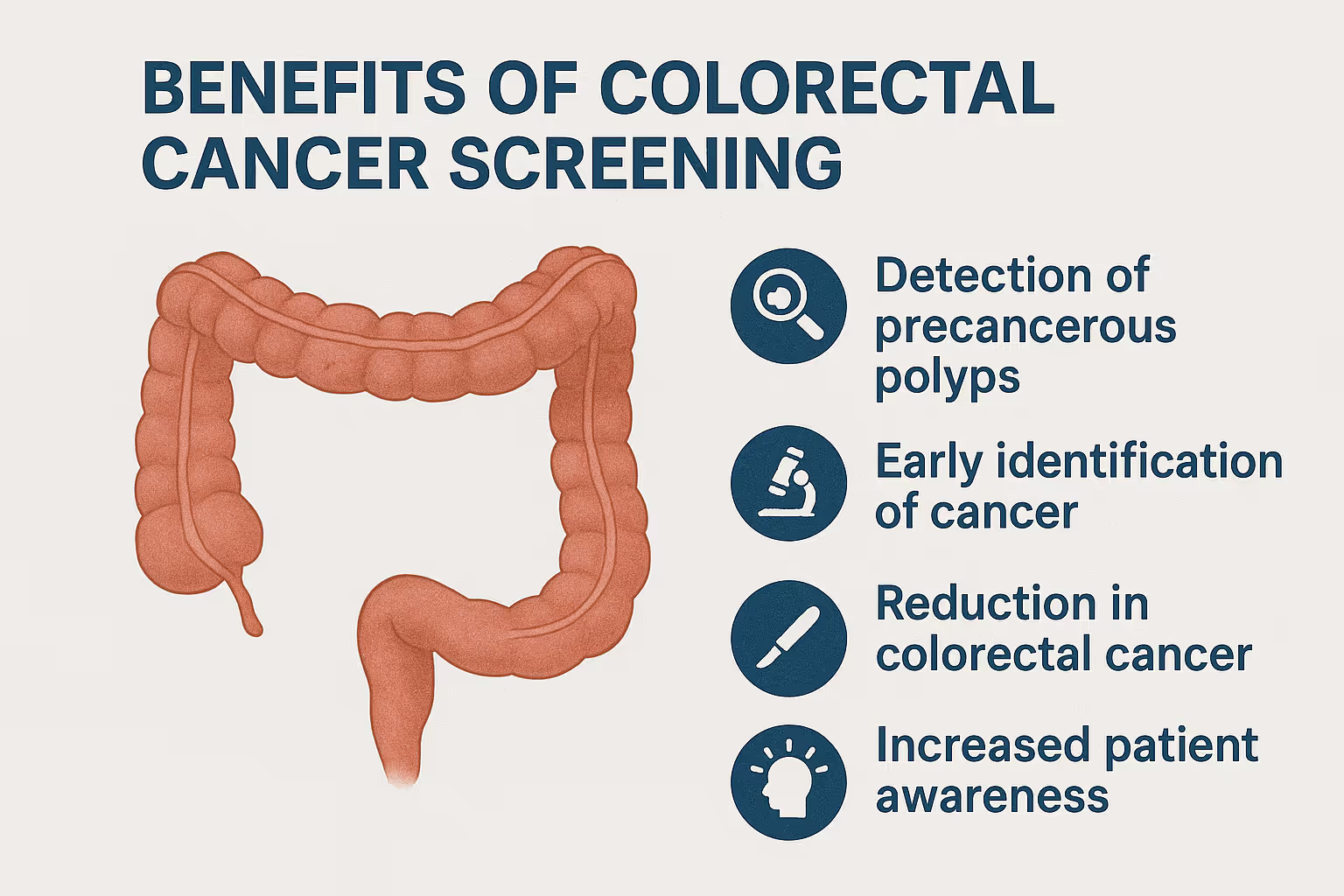
What are the benefits of colorectal cancer screenings?
Colorectal cancer screenings provide significant medical and economic advantages by detecting disease early and preventing its progression. These screenings not only save lives but also reduce the burden on the healthcare system by catching issues before they become more complex or costly to treat. Key benefits of colorectal cancer screenings include:
- Early detection of colorectal cancer allows for timely treatment when outcomes are most favorable.
- Removal of precancerous polyps prevents them from developing into cancer.
- Reduction in the number of new colorectal cancer cases through the proactive identification of abnormal tissue.
- Decreased mortality rates, as early-stage cancers are far more treatable than advanced-stage disease.
- Lower treatment costs, as early intervention typically avoids expensive procedures or extended hospital care.
- Improved quality of life, by preventing advanced disease and reducing the need for aggressive treatment later.
- Increased survival rates, as early-stage colorectal cancer has a 5-year survival rate of over 90% when treated promptly.
The American Cancer Society recommends initiating regular screenings at age 45 for those at average risk. Maintaining consistent screening schedules is a proven strategy for cancer prevention and long-term health.
How effective are colorectal cancer screening tests?
Colorectal cancer screening tests are highly effective tools for reducing both the incidence and mortality of colorectal cancer. They help individuals by detecting cancer at an early stage, often before symptoms appear, when it is most treatable and the chances of recovery are significantly higher.
These tests also play a critical preventive role by identifying and removing precancerous polyps before they turn into cancer. This dual function of early detection and prevention makes screening a cornerstone of long-term colorectal health.
By catching cancer early, screening tests greatly reduce the need for aggressive treatments like chemotherapy or surgery, improving patient quality of life and reducing healthcare costs. According to the American Cancer Society, regular screening can lower the risk of dying from colorectal cancer by up to 68%.
Overall, screening tests for early disease detection serve as one of the most powerful tools in public health, saving lives, minimizing suffering, and promoting timely intervention when it matters most.
When should colorectal cancer screening for colon cancer be started?
Colorectal cancer screening should begin at age 45 for individuals at average risk. This guideline is based on updated research showing an increasing number of colorectal cancer cases in adults under 50. Starting screening at 45 allows for early detection of precancerous polyps and asymptomatic cancers, when treatment is more effective and less invasive. Early intervention not only improves survival rates but also helps prevent cancer from developing altogether. For individuals with higher risk factors, such as a family history of colorectal cancer or certain genetic conditions, screening may need to begin even earlier based on medical advice.