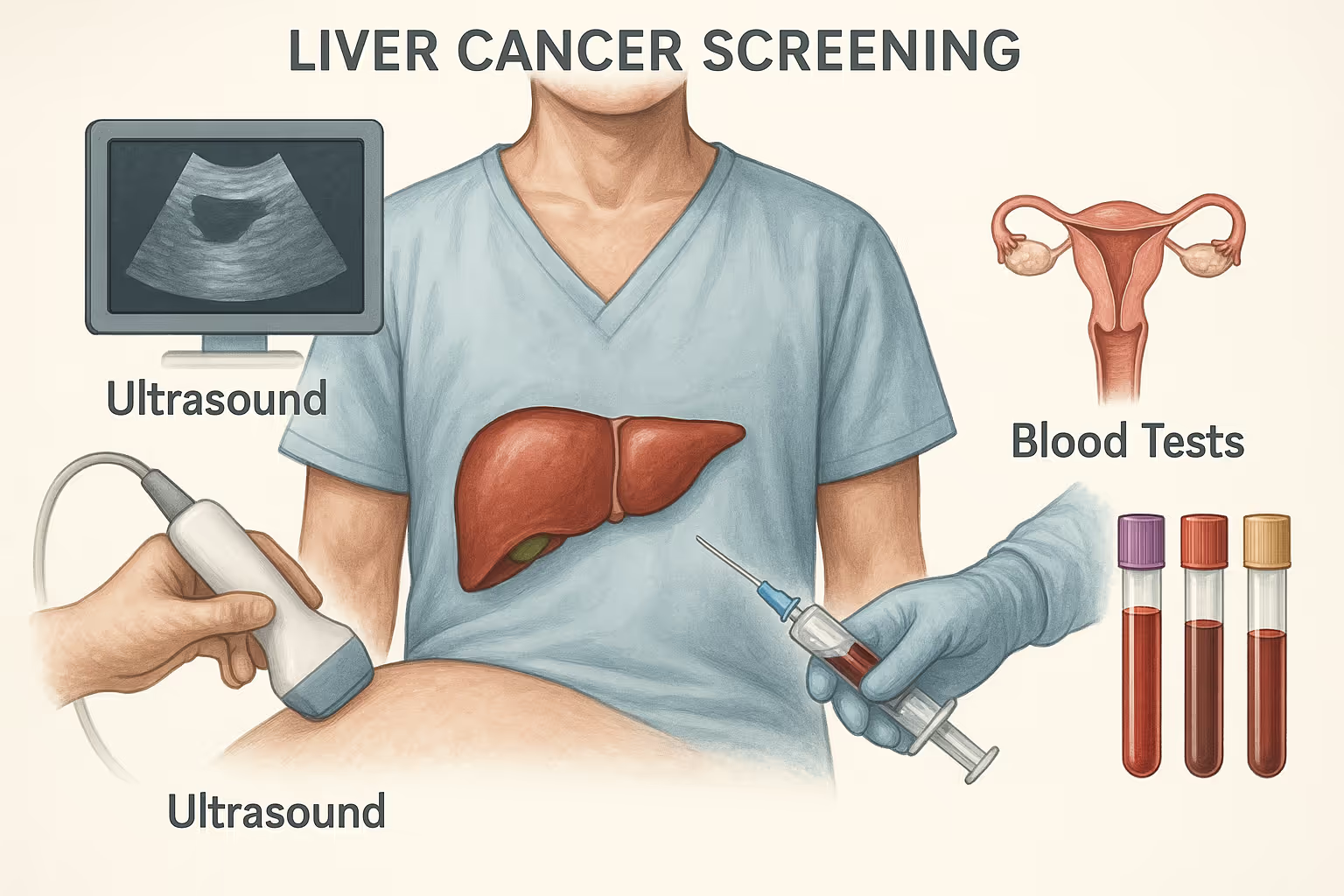
Liver cancer screening is a preventive health measure designed to detect cancer at an early stage, often before symptoms appear. It is especially important for individuals with chronic liver conditions such as hepatitis B or C, cirrhosis, or a family history of liver cancer. The screening process typically involves a combination of medical tests, most commonly abdominal ultrasound, alpha-fetoprotein (AFP) blood test, and, when necessary, advanced imaging like CT or MRI scans. These tools work together to evaluate liver structure and function for any early signs of hepatocellular carcinoma.
Clinical guidelines recommend that high-risk individuals begin routine screenings at specific ages, with testing repeated every six months to ensure timely detection. Costs for these tests can range from $50 for basic blood work to over $3,000 for advanced imaging, depending on location and insurance coverage. By identifying cancer early, liver cancer screening not only improves treatment outcomes and survival rates but also supports a healthier lifestyle through consistent monitoring and proactive care. Regular testing empowers individuals to make informed health decisions that can significantly reduce complications and improve their longevity.
Key Takeaways
- Liver cancer screening is crucial for high-risk individuals and typically involves imaging and blood tests to detect cancer early and improve survival rates.
- The combination of abdominal ultrasound and Alpha-Fetoprotein (AFP) blood test is considered the most effective screening method for liver cancer.
- Screening guidelines recommend regular tests based on individual risk factors, with costs for screening varying widely depending on the procedure and location.
What is liver cancer screening?
Liver cancer screening is a preventive health strategy that uses medical tests to detect liver cancer at an early stage, often before symptoms appear. It is primarily recommended for individuals at high risk, including those with chronic hepatitis B or C, liver cirrhosis, or a family history of liver cancer.
The screening process typically involves two main components: imaging tests, such as abdominal ultrasounds, and blood tests, like the alpha-fetoprotein (AFP) test. Imaging helps visualize the liver for structural abnormalities, while blood tests detect tumor markers associated with liver cancer. These tests are repeated at regular intervals to monitor changes over time.
The purpose of liver cancer screening is to identify hepatocellular carcinoma (HCC), the most common type of primary liver cancer, at a stage when it is still treatable. Early detection allows for more treatment options, better survival rates, and improved long-term outcomes.
How effective are liver cancer screening tests?
Liver cancer screening tests are highly effective in detecting cancer at an early, more treatable stage, especially in high-risk individuals such as those with hepatitis B, hepatitis C, or cirrhosis. Studies have shown that regular screening can significantly increase survival rates by identifying hepatocellular carcinoma before symptoms develop, when treatment options are more effective and less invasive.
Beyond clinical effectiveness, screening is also a gateway to a healthier lifestyle. It prompts individuals to remain aware of their liver health, adhere to follow-up care, and adopt healthier habits. By enabling early action and reducing uncertainty, liver cancer screening not only improves longevity but also supports proactive health management that contributes to overall wellness.
Personalized liver health monitoring with Fountain Life
For individuals who want to take a proactive, precision-based approach to cancer prevention, Fountain Life offers advanced screening programs that go beyond traditional care. By combining AI-backed diagnostics with whole-body imaging and real-time biomarker analysis, Fountain Life helps detect liver abnormalities at their earliest stages, often before standard symptoms appear. This level of insight supports timely medical decisions and long-term liver health management for high-risk individuals.
What tests are involved in Liver cancer screening?
Liver cancer screening tests are medical procedures used to detect liver cancer early by evaluating both the structure and function of the liver. These tests are especially important for high-risk individuals and are designed to identify abnormalities before symptoms appear.
The screening process typically includes a combination of imaging and blood tests. Each test plays a unique role, and together they provide a more accurate and complete assessment of liver health. The main tests involved in liver cancer screening include:
- Abdominal Ultrasound: A non-invasive imaging test that uses sound waves to visualize the liver and detect tumors or irregularities.
- Alpha-Fetoprotein (AFP) Blood Test: A blood test that measures levels of AFP, a protein that may be elevated in people with liver cancer.
- Computed Tomography (CT) Scan: A high-resolution imaging method that creates detailed cross-sectional views of the liver to identify tumors and assess their size and spread.
- Magnetic Resonance Imaging (MRI): In some cases, an MRI may be used to provide enhanced images of liver tissue for further evaluation.
Using these tests in combination improves the likelihood of early detection and accurate diagnosis, forming the foundation of an effective liver cancer screening strategy.

1. Abdominal ultrasound
Abdominal ultrasound is a non-invasive imaging test that uses sound waves to produce real-time images of the liver. It is the primary method used for liver cancer screening because it is safe, widely available, and cost-effective. This test is effective at detecting early liver tumors, particularly in high-risk individuals such as those with chronic hepatitis B or C and liver cirrhosis. However, its sensitivity may be reduced in individuals with obesity or fatty liver. Clinical guidelines recommend an abdominal ultrasound every six months for high-risk populations. Men with hepatitis B should begin screening at age 40, women at age 50, and individuals of Asian or African descent may require earlier screening. During the procedure, a technician applies a gel to the patient’s abdomen and moves a handheld device over the area to generate images, making it a quick and painless process. The estimated cost for an abdominal ultrasound typically ranges from $300 to $600, depending on the facility and geographic location.
2. Alpha-fetoprotein (AFP) blood test
The AFP blood test measures the level of alpha-fetoprotein, a protein that can be elevated in individuals with liver cancer. It is a supportive test that adds diagnostic value when used alongside imaging, like ultrasound. While not as accurate on its own, since AFP levels can also rise due to cirrhosis or hepatitis, it becomes more effective when combined with imaging, particularly in detecting hepatocellular carcinoma. It is not the primary test,t but remains an important component of a complete screening strategy. Guidelines recommend combining AFP testing with ultrasound every six months for high-risk individuals. The test involves drawing a small sample of blood from a vein and sending it to a lab for analysis. There is no preparation needed, and the process is quick and minimally invasive. The estimated cost for an AFP test typically falls between $50 and $200, depending on the lab and whether additional blood panels are included.
3. Computed tomography (CT) scan
A CT scan uses multiple X-rays taken from different angles to create cross-sectional images of the liver. It is highly effective in identifying liver tumors, their size, and whether they have spread to surrounding tissues. CT scans are more sensitive than ultrasound for detecting small or deeply located tumors, especially in patients with cirrhosis. While not the first-line screening tool due to its cost and radiation exposure, it is commonly used for further evaluation when ultrasound results are inconclusive or when tumors are suspected. There are no universal screening guidelines for routine CT use, but it is often recommended by specialists based on individual patient history and risk. CT scans are typically initiated when patients present with abnormal ultrasound or AFP findings. The process involves the use of a contrast dye and takes about 15–30 minutes in a hospital or imaging center. The estimated cost of a liver CT scan ranges from $1,000 to $3,000, depending on the facility, whether contrast is used, and insurance coverage.
4. Magnetic resonance imaging (MRI)
MRI uses powerful magnets and radio waves to produce highly detailed images of the liver without radiation. It is particularly useful for characterizing liver lesions that are unclear on ultrasound or CT scans. MRI is very effective in distinguishing between benign and malignant liver tumors, making it a valuable diagnostic tool for follow-up. However, due to higher cost and limited availability, it is not used as a routine screening method but rather for confirmation or further investigation. There are no specific guidelines recommending MRI as a primary screening tool, but it may be employed when ultrasound or CT results are ambiguous. MRI can be started at any age depending on clinical necessity. The test takes 30–60 minutes, and patients may receive a contrast agent through an IV for enhanced imaging. It is non-invasive but may not be suitable for individuals with certain implants or severe claustrophobia. The estimated cost of a liver MRI typically ranges from $1,200 to $4,000, depending on the complexity and location of the imaging center.
Can you perform a liver cancer screening test at home?
No, liver cancer screening cannot be reliably performed at home. These tests involve advanced imaging technologies, such as ultrasound, CT scans, or MRI, that require specialized equipment and trained medical professionals to operate and interpret. Additionally, blood tests like the alpha-fetoprotein (AFP) test must be processed in certified laboratories to ensure accurate results. Without access to professional diagnostic tools and clinical oversight, attempting liver cancer screening at home poses serious risks, including missed diagnoses or false reassurance. Although home testing may offer convenience and privacy, it lacks the precision and safety required for detecting a condition as serious as liver cancer. Ultimately, only clinical settings can deliver the level of accuracy and early detection needed to ensure effective treatment outcomes.
What is the best screening test for liver cancer?
The best and most effective screening test for liver cancer is a combination of abdominal ultrasound and the alpha-fetoprotein (AFP) blood test. This dual approach is considered the gold standard for early detection, especially in high-risk individuals. The abdominal ultrasound allows healthcare providers to visualize the liver and identify any structural abnormalities or tumors, while the AFP blood test measures protein levels in the blood that may be elevated due to liver cancer.
This combination is superior because it addresses both structural and biochemical indicators of hepatocellular carcinoma, increasing the chances of detecting cancer at an early, more treatable stage. Ultrasound alone may miss small or deep tumors, and AFP levels can be elevated due to non-cancerous liver conditions. However, when used together every six months as part of a regular screening schedule, they offer a more accurate and reliable method for early intervention and improved survival rates.
Can you detect liver cancer with a blood test?
Yes, liver cancer can sometimes be detected with a blood test, specifically the alpha-fetoprotein (AFP) test. AFP is a protein that may be elevated in people with hepatocellular carcinoma, the most common type of liver cancer. However, the AFP test alone is not definitive—some individuals with liver cancer may have normal AFP levels, while others with chronic liver diseases like hepatitis or cirrhosis may show elevated levels without having cancer. For this reason, the AFP blood test is most effective when used in combination with imaging tests, forming a more reliable screening strategy.
Can you detect liver cancer with an abdominal ultrasound?
Yes, abdominal ultrasound is one of the primary tools used to detect liver cancer, especially in its early stages. This non-invasive imaging test uses sound waves to produce real-time images of the liver, allowing healthcare providers to identify tumors, nodules, or other abnormalities. It is particularly effective in high-risk patients when performed regularly, typically every six months. While very useful, the accuracy of ultrasound may be limited in patients with obesity or advanced cirrhosis, and it may not detect very small or deep tumors. Therefore, it is often paired with blood tests to improve diagnostic accuracy.
Can you detect liver cancer with an X-ray?
No, a standard X-ray is not effective for detecting liver cancer. X-rays are limited to imaging bones and dense tissues, and they do not provide the detail necessary to visualize liver tumors or distinguish between healthy and cancerous liver tissue. Unlike more advanced imaging techniques such as CT scans or MRIs, X-rays cannot capture the internal structure or soft tissue contrast needed to identify hepatocellular carcinoma. As a result, X-rays are not used in liver cancer screening or diagnosis.
Can you detect liver cancer with a CT scan?
Yes, a CT scan can effectively detect liver cancer by providing high-resolution, cross-sectional images of the liver. It allows physicians to identify tumors, assess their size and location, and evaluate whether the cancer has spread to nearby structures. CT scans are particularly valuable when ultrasound results are inconclusive or when more detailed imaging is needed for diagnosis or treatment planning. In many cases, a contrast-enhanced CT scan is used to improve the visibility of liver lesions. While not recommended as a routine screening tool due to cost and radiation exposure, it plays a crucial role in confirming and staging liver cancer.
What guidelines should you follow for screening liver cancer?
Liver cancer screening guidelines are structured recommendations aimed at detecting cancer early in individuals at increased risk. These guidelines help clinicians determine who should be screened, which tests to use, when to start, and how often to repeat them. The purpose is to catch hepatocellular carcinoma (HCC) in its early stages, when treatment is most effective and outcomes are significantly better.
- Screen individuals with chronic hepatitis B or C, liver cirrhosis, or a family history of liver cancer.
- Use abdominal ultrasound combined with the alpha-fetoprotein (AFP) blood test as the standard screening method.
- Conduct liver cancer screening every 6 months for those in high-risk categories.
- Begin screening at age 40 for men with chronic hepatitis B.
- Begin screening at age 50 for women with chronic hepatitis B.
- Start screening earlier for Asian or Pacific Islander individuals with hepatitis B, based on physician assessment.
- Begin screening at age 20 for men from sub-Saharan Africa with chronic hepatitis B due to elevated risk.
- Initiate immediate screening for individuals with cirrhosis, regardless of age or cause.
- Screen patients co-infected with HIV and hepatitis B or C regularly once chronic infection is confirmed.
- Consider screening for individuals with other risk factors such as autoimmune hepatitis, hemochromatosis, or alpha-1 antitrypsin deficiency based on liver fibrosis stage.
Following these guidelines helps identify liver cancer early, enabling timely intervention and improving survival outcomes.

At what age should you perform screening for liver cancer?
The age at which liver cancer screening should begin depends on a person’s risk factors. For men with chronic hepatitis B, screening is recommended starting at age 40. For women with chronic hepatitis B, the recommended starting age is 50. However, individuals of Asian or Pacific Islander descent with chronic hepatitis B may need to begin screening earlier, depending on clinical judgment. Men from sub-Saharan Africa who are chronically infected with hepatitis B should start routine screening as early as age 20 due to their significantly higher risk.
Patients with liver cirrhosis, regardless of its cause, should begin screening immediately, regardless of age. Similarly, individuals co-infected with HIV and hepatitis B, C, or D require regular screening from the time of diagnosis. Those with a family history of liver cancer or other chronic liver diseases should also follow early and consistent screening protocols. These age-specific recommendations are designed to ensure that high-risk individuals are monitored appropriately and diagnosed at the earliest possible stage.
What is the cost of screening for liver cancer?
The cost of liver cancer screening depends on the type of test performed, the healthcare facility, geographic location, and whether or not insurance coverage applies. On average, an abdominal ultrasound, the primary imaging test used in routine screening, costs between $300 and $600. A blood test for alpha-fetoprotein (AFP), which is commonly combined with ultrasound, typically costs around $50 to $200. If further imaging is needed, a CT scan may cost $1,000 to $3,000, while an MRI can range from $1,200 to $4,000, depending on the level of detail required and use of contrast agents.
These costs generally include the procedure itself, the radiologist’s or laboratory’s interpretation, and facility fees. Additional charges may apply if follow-up imaging, consultations, or biopsies are recommended based on the results. Other influencing factors include the complexity of the test, whether contrast is used, the qualifications of the provider, and whether the patient pays out of pocket or through insurance. Patients should confirm coverage with their insurance provider and explore available financial assistance programs, especially if they fall into high-risk groups requiring regular screening.

Access advanced diagnostics through Fountain Life
While standard liver screening can be costly and vary in quality, Fountain Life provides access to comprehensive and accurate diagnostics through its membership model. The screenings are performed in state-of-the-art facilities with expert teams, ensuring not only early detection but also personalized guidance on next steps. For those seeking high-value, data-driven care, Fountain Life eliminates the guesswork and empowers you to take control of your health journey.
Is liver cancer screening cost covered by insurance?
Yes, liver cancer screening is often covered by insurance, especially for individuals classified as high-risk. However, coverage is not universal and can vary depending on the insurance provider, plan type, and state regulations. While the Affordable Care Act mandates coverage for several preventive services, liver cancer screening is typically covered only when it is considered medically necessary, such as for individuals with chronic hepatitis B or C, cirrhosis, or a family history of liver cancer.
Some states also have specific laws requiring private insurers to cover cancer screenings, which may include liver cancer in certain cases. Patients are strongly encouraged to verify their coverage directly with their insurance provider before scheduling tests. For uninsured or underinsured individuals, various local programs and nonprofit organizations may offer free or low-cost screening services, ensuring that financial barriers do not prevent access to timely cancer detection.
Are there any free liver cancer screenings?
Yes, free liver cancer screenings are available in some regions, especially for high-risk individuals. Programs like the British Liver Trust’s mobile liver scan clinics in the UK, government-supported services in Pakistan (e.g., Sehat Sahulat Program), and community health initiatives in the U.S. occasionally offer no-cost screening services. These programs aim to improve early detection by making preventive care accessible to underserved or high-risk populations. Availability may vary by location, so individuals should check with local health organizations or public hospitals.
What are the benefits of liver cancer screening tests?
Liver cancer screening tests are essential preventive tools designed to detect cancer at its earliest stages, especially in individuals with known risk factors. These tests offer multiple medical and lifestyle-related benefits that support early intervention, better outcomes, and long-term health management. Key benefits include:
- Early detection of cancer: Liver cancer can be identified before symptoms appear, which significantly improves treatment success rates and survival.
- Increased treatment options: When liver cancer is found early, patients have access to a wider range of curative treatments, including surgery, ablation, and transplant.
- Improved survival rates: Early-stage hepatocellular carcinoma responds better to treatment, leading to longer life expectancy and reduced cancer-related mortality.
- Better disease monitoring: Regular screening helps monitor underlying liver conditions such as cirrhosis or hepatitis, allowing timely adjustments in treatment plans.
- Reduced healthcare costs over time: Detecting liver cancer early can help avoid the high costs associated with managing late-stage disease, including hospitalization and intensive care.
- Health behavior improvement: Routine screenings often lead to increased patient awareness, encouraging healthier lifestyle choices such as reducing alcohol use, improving diet, and managing weight.
- Peace of mind: Regular checkups can provide reassurance for high-risk individuals, reducing anxiety and enabling more proactive health management.
Does liver cancer screening test save lives?
Yes, liver cancer screening tests can save lives, especially when used consistently in high-risk populations. Research has shown that regular screening with abdominal ultrasound and alpha-fetoprotein (AFP) blood tests significantly increases the chances of detecting hepatocellular carcinoma (HCC) at an early stage. Early-stage liver cancer is more likely to be treated successfully with curative interventions such as surgical resection, liver transplantation, or local ablation therapies.
According to a study published in Hepatology, biannual screening in patients with cirrhosis was associated with a 37% reduction in liver cancer-related mortality. Another study in Clinical Gastroenterology and Hepatology found that early detection through routine screening nearly doubled the five-year survival rate compared to late-stage diagnosis. These findings support clinical guidelines that recommend routine liver cancer screening in high-risk groups, emphasizing that timely detection directly impacts life expectancy and treatment success.
How to maintain a healthy life with proper liver cancer screening tests?
Proper liver cancer screening plays a critical role in maintaining overall health, particularly for individuals with chronic liver conditions or a family history of liver cancer. By detecting liver abnormalities early, screening enables timely medical intervention that can prevent the progression of cancer and reduce the risk of complications. This proactive approach not only improves treatment outcomes but also encourages individuals to stay informed and engaged in their health. Routine screening often leads to increased health awareness, prompting better lifestyle choices such as maintaining a balanced diet, avoiding alcohol, exercising regularly, and managing weight. Over time, these habits contribute to reduced liver stress and lower the likelihood of disease recurrence. Most importantly, consistent screening can significantly improve your longevity by catching life-threatening conditions early, allowing for effective management and a better quality of life.